Neck surgery
Read our guide below about having neck surgery.
You can also download a PDF version of this patient information by following the link on the right.
This information will help you understand:
- what will happen when you have your neck operation
- how you can help yourself to recover as quickly as possible.
The information may vary according to your individual situation. It will answer some of the questions you may have.
If there’s anything you and your family aren’t sure about, contact your consultant or an appropriate healthcare professional.
About your spine
Your neck or cervical spinal column has squares of bone (vertebrae) stacked on top of each other with shock absorbers (discs) in between them. The spinal cord sits behind this, lying in a hole through the centre with nerves coming off it to your arms and legs.
Joints and more bone, where muscles and ligaments attach, lie behind the spinal cord protecting it from behind.

Illustration of the spine showing bones and discs
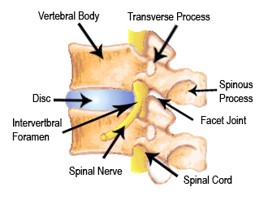
Diagram of the neck showing discs, joint and spinal cord
Why am I having spinal surgery?
We usually do neck operations to remove pressure on the nerves that go down your arm and on the spinal cord.
Pressure on the nerves in your neck can cause arm pain (cervical radicular pain or radiculopathy), weakness, tingling or numbness. You may struggle with using your arm.
Pressure on your spinal cord can cause damage to the cord (myelopathy). Your symptoms might include:
- numb, clumsy hands (pins and needles)
- heavy legs feelings
- an inability to walk at a fast pace
- balance issues like stumbling or unsteadiness as if you’re drunk
- inability to write with a pen, grip or button a shirt
- intermittent electric shock type of pains in your arms and legs especially when you bend your head forward.
As part of the normal ageing process soft tissues and bones in your neck may harden and become thickened. Over time, the discs lose water and sometimes bulge. These changes together can narrow the central passageway where the nerves and the spinal cord pass through.
As the narrowing worsens, the cord can be compressed and damaged (myelopathy) and cause arm symptoms and problems with your balance or walking, and hand function.
Central stenosis means narrowing of the central canal where the spinal cord lies.
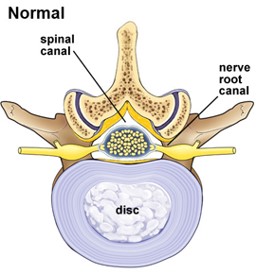
Diagram showing a normal neck
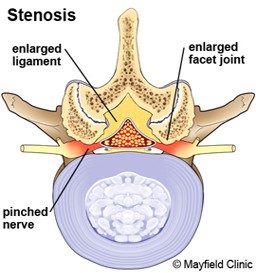
Diagram showing stenosis in the neck
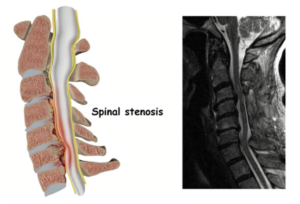
Image of spinal stenosis
How will surgery help?
Taking the pressure off your nerves will help relieve and improve your symptoms. Good relief from arm pain after surgery usually happens in around 85 to 90% of cases (9 out of 10 people).
Surgery can also help with cervical myelopathy. It’s a serious ongoing condition and the damage to the cord can continue without surgery. Taking the pressure off the spinal cord helps to stop the damage and weakness getting worse. It also helps to keep the current muscle and nerve function.
Relief from neck pain is more difficult to predict and is not the main aim of the surgery.
What type of surgery might I need?
Treatment for cervical myelopathy is called decompression surgery. It makes more space around the nerve and spinal cord by removing bone or disc material. Surgery stops further damage to the spinal cord and reduces loss of using your arm and walking.
The surgeon removes the tissues (disc or bone) pressing on the nerve and spinal cord. There are no gaps left in the spine. Modern techniques mean that healing takes place very quickly and once it’s healed the neck feels stronger.
As you get older, the discs between the vertebrae get less plump and bulge. Despite the term ‘slipped disc’, the disc doesn’t slip in and out but some of the disc material can stick out and pinch a nerve. It’s also called a herniated disc.
In most cases the body will reabsorb this material and heal itself. Sometimes this doesn’t happen. The bulge may be near a nerve and large enough to push on it causing arm pain, pins and needles, numbness or weakness.
Discectomy surgery involves removing the piece of disc pressing on the nerve to reduce the arm pain caused by the pinched nerve.
The arm pain doesn’t always improve immediately after surgery but can improve over a period of time, often months, as the nerve recovers.
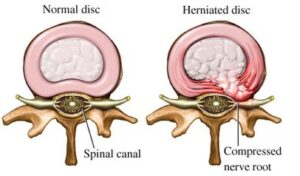
Diagram of a normal and herniated disc
For discectomy and decompression surgery, you’ll have a general anaesthetic so you’re fully asleep. We can also do both surgeries in one operation.
There are different techniques used to remove the pressure from the nerves and the spinal cord. The way we approach the cervical spine can differ from either the front (anterior) or back (posterior) of the neck. The choice of approach will depend on where most pressure on the nerve comes from.
This surgery removes the problem disc.
We do the surgery through the front of your neck to access the disc causing pressure on the verve, usually on the right hand side where we cut one small muscle.
Once we remove the disc, we replace it with a metal or synthetic implant to help keep the vertebrae together. Sometimes we do a bone graft usually taken from your pelvis. These two bones will grow together (called fusion) so there’s complete loss of movement at the level of the operation.
Occasionally, we use plates and screws to improve stability.
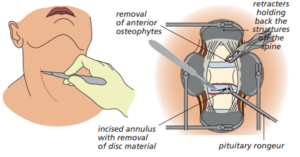
Diagram showing the process involved with ACDF surgery
This surgery removes the problem disc. The procedure is very similar to ACDF and your surgeon goes through the front of your neck to remove the disc pinching on the nerve. An artificial disc goes into the space where the surgeon removes the disc.
This metal implant helps to maintain movement between the two vertebrae and avoids the need for fusion.
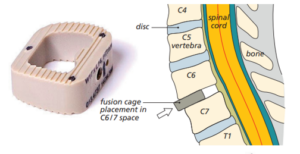
Diagram showing the cage or implant to keep the vertebrae together
This type of surgery happens when:
- stenosis is due to more than just the disc problem
- there’s more than one level that has narrowing
We do the surgery through the front of your neck. The surgeon removes the disc and the vertebral body (bone) to make room for the spinal cord and nerves. They replace the vertebrae with a vertebral body cage or sometimes a solid piece of bone graft. They may put a metal plate on the front of your spine to add stability and stop the cage or graft from moving out of place.
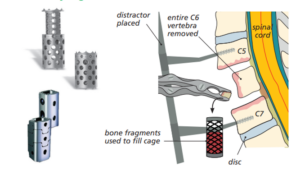
Diagram showing the removal of the vertebrae
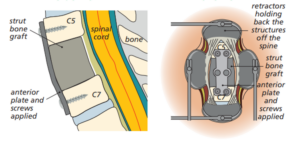
Diagram showing a bone graft with plates and screws to add stability
We do this operation from the back of your neck.
Your head and neck are kept still and suspended securely over the operating table using a special clamp applied temporarily to your skull with pins. The surgeon removes the back of your vertebrae that covers the spinal canal (lamina). This increases the space and takse away the pressure on the spinal cord or nerves, allowing the nerves to ‘float backwards.’
We do this surgery because of many levels of narrowing. This is because of bone growing into the space for the nerves or ‘thickened’ ligaments on the bony arch at the back of the neck.

Picture showing the process involved with a cervical laminectomy
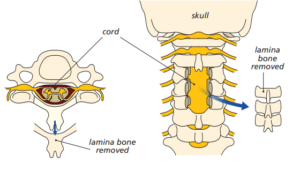
Diagram showing the removal of the lamina bone
Removing the cervical lamina completely can cause problems with the stability of the cervical spine. Your surgeon may add stability to the spine by placing a rod on the side of your spine and attach it with screws.
With a similar approach to cervical laminectomy, your surgeon will partly cut the lamina bone on one side and completely cut on the other. They’ll rotate the lamina bone to an open position like opening a door.
Your surgeon will hold the bone in the open position using small metal plates and screws like a hinge. The metalwork connects the same bone back to itself but in a new position. These techniques increase the space for the spinal cord and take the pressure off it.
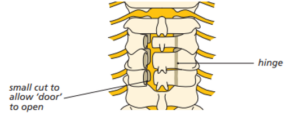
Diagram showing the process for a cervical laminoplasty
What are the possible risks or complications of surgery?
These might include the following.
Deep infection
This happens in around 1 in every 100 cases. You’ll usually have antibiotics into a vein at the time of surgery to reduce this risk.
Superficial wound infections
4 in every 100 patients get this and may need a short course of antibiotics.
Bleeding
Less than 1 in every 100 patients have a major bleed which may need treatment.
Durotomy (damage to the dura)
The dura is the delicate sac that contains the spinal nerves inside the spinal canal. Occasionally, around 1 in 25 cases, this can get snagged or torn accidentally during the surgery.
We can usually repair the dura at the time and it won’t cause any long term problems. You might have a headache for a couple of days afterwards.
Blood clots
These may happen in the deep veins in your legs or lungs. We’ll give you surgical stockings and pumps on your legs during surgery to reduce this risk.
Sensory change or muscle weakness in arms
This is uncommon and may happen in around 1 in 100 cases due to nerve root damage. It’s usually temporary but sometimes can be long-term. Problems with nerve function in up to 31% of patients are mostly temporary.
Post-op bladder or bowel dysfunction
The risk of damage to the nerves that supply your bladder and bowel is very rare (1 in 1,000 cases).
Repeat surgery
1 in every 100 patients have more back surgery during the 10 years that follow neck surgery. This is because of ongoing wear and tear changes elsewhere in your spine.
Age
For elderly patients some risks increase slightly. These include:
- blood clots
- heart attacks
- urine/chest infection
- heart failure.
Return of pain
In less than 1 to 5 in 100 people, the natural process of healing by scar tissue causes pain to return by covering the nerves in too much scar tissue. Physiotherapists can treat this. In some cases you may need a referral to the pain team after surgery.
Temporary damage
This can happen in up to 1% of patients and include:
- blood vessel damage
- urinary tract infection
- urinary retention
- vertebral fracture.
Digestion problems
These can affect up to 7% of patients.
Problems with metal work used in surgery
This may involve breaking screws or rods, or the bone failing to heal around the metal leading to movement of the screws. This may or may not need further surgery in the future. Problems with the cage supporting the vertebrae, or the bone graft affect 5 out of 100 cases.
Complications from taking a bone graft from the pelvis
This might include graft site pain and damage to the sensory nerve supplying sensation to front of your thigh.
Pain from other areas in the neck
This can happen in the long term or in years to come,
Positioning during surgery
In rare cases this can cause:
- pressure problems
- skin and nerve injuries
- eye problems (very rarely blindness).
We use special operating tables to reduce these risks. Shoulder problems and upper limb nerve problems are also a risk.
Are there any serious complications?
Yes but these are very rare.
Damage to the spinal cord can result in paralysis or loss of bowel and bladder function. This can happen due to bleeding into the spinal canal after the surgery (a haematoma). We make every effort to reverse this by returning to surgery to wash out the haematoma, but can’t guarantee recovery of the nerve damage.
Stroke, heart attack or other medical or anaesthetic problems can also happen.
General anaesthetic fatal complications have been reported in 1 out of 250,000 cases. Death, although extremely rare has also been reported in 1 out of 250,000 cases under general anaesthetic.
Specific risks associated with anterior surgery (ACDF, ACD-R and corpectomy)
These risks relate to surgeries where the surgeon does the operation from the front of your neck.
Stroke
There’s a slight risk of injury to the vertebral artery (blood vessel) that runs along the side of the spine. This can happen when the surgeon removes the cervical vertebral body and could lead to stroke and/or life threatening bleeding.
Bleeding in the wound and swelling in the windpipe
This can cause difficulty in breathing or swallowing. It’s rare but if it happens you may need to go back to the operating theatre to stop the bleeding.
Bone graft/cage/artificial disc movement
This can happen in 2 out of 100 cases and you may need another. In very rare cases, movement can cause severe damage and paralysis.
Damage to the windpipe (trachea) or food pipe (oesophagus)
This happens in fewer than 1 in 100 cases.
Injury to the small nerve that supplies the vocal cords
This can cause:
- temporary hoarseness of the voice
- permanent, but rare hoarseness of the voice
- temporary strained and uncomfortable swallowing.
You may need to eat soft food for a few days.
Droopy eyelid
This can happen in 1 in 100 patients. It’s not usually obvious and nearly always improves.
What can I do to prepare for surgery?
It’s important to look after yourself by syating healthy, eating a well balanced diet and keeping your weight down.
If you smoke, you must stop or at least cut down. Get advice from the pre-operative assessment department through their ‘live well, stay well’ campaign.
You should also:
- ask questions about the procedure and know what you’re signing on the consent form
- make plans for your recovery at home following surgery.
This may include telling your employer, making sure you have a care package if you’ll help and having someone ready to take you home when we discharge you. Make sure you plan for meals, childcare and carers..
What will happen before my operation?
We’ll send you an appointment for a pre-operative assessment. This involves a general health check to make sure you’re fit for surgery. A nurse will do blood and urine tests, x-rays and any other tests we may need.
We’ll also ask you about any medications you’re taking including herbal medicines. Please bring your medicines, or a full list of your current medication with you to the pre-operative assessment appointment.
Plan for a half day at your appointment. You can bring a family member or someone else with you. There’s a hospital cafeteria on site for drinks and food.
You must tell us about any changes to your medication or health before your operation.
We’ll tell you before your operation when to stop eating and drinking.
What do I need to bring with me to hospital when I come for my operation?
You’ll need to stay in hospital so make sure you bring toiletries, night clothes, medication and any small electronic devices you may need.
See our list of recommended things to bring with you.
What will happen on the day of surgery?
Your anaesthetist will assess you before surgery. They may ask if you have a preference for a local or a general anaesthetic. The anaesthetist will make the final decision about the type that’s best for you based on
- your preference
- the type of operation you’re having
- your general condition
- any previous experiences you’ve had with different anaesthetics.
When you arrive in the anaesthetic room, the operating theatre staff will check your notes and ask you more questions. Don’t be alarmed if several people ask you the same questions.
What happens after surgery?
We’ll take you to the recovery room where a nurse will monitor your progress. They’ll:
- check your breathing, pulse, temperature and blood pressure
- ask how you feel
- ask you to take deep breaths
- check the circulation and sensation in your legs and feet
- ask and assess if you have any pain.
What will happen while I’m in hospital?
From the recovery room, we’ll take you to the orthopaedic ward where we’ll look after you for the rest of your stay.
You may return from theatre with a urinary catheter if needed. We’ll remove this as soon as you can walk to the toilet.
Intravenous fluids and oxygen
You may have intravenous fluids or a patient controlled analgesia (PCA) which gives you pain relief through a drip until you’re comfortable. This isn’t done regularly. You may need oxygen through a mask or nasal tubing. Very uncommonly, you may also have a drain on your wound.
Collar
You may need a soft or hard collar after your operation. This will depend on what type of operation you had. Your surgeon will recommend which collar is best and how long to use it for. Most of the time, it’s only for comfort and extra support. You should use it less as you get more comfortable and your pain feels more controlled.
On the ward the nurses will check your breathing, pulse, temperature and blood pressure. They’ll check the dressings applied to your incision and the drain if you needed it.
What can I expect after my operation?
If your pain is under control, you should be able to sit up in bed and walk to the toilet with assistance. A physiotherapist will show you exercises, explain how to increase your mobility and get back to normal.
The physiotherapist will also check you can walk safely and manage stairs if necessary. When they feel it’s safe for you to walk, you can go home. This can be the same day as your surgery or the following day.
If you stay in hospital over 24 hours, a pharmacist will visit the ward to check your medication is right for you. They can answer any questions about your medication.
Your arm pain might go immediately after the operation. Sometimes it may take up to 8 weeks or longer to go as the nerve needs time to recover from the pressure it had on it. You may still need to take pain killers or neuropathic medication. It’s important to slowly stop using them.
The wound may be a little sore and we’ll give you pain relief for this. The soreness will go in a few days.
If you had cervical myelopathy
This type of myelopathy involves compression of the spinal cord in the neck. If you had surgery for cervical myelopathy, any improvement in hand function or walking ability may be slight and can happen slowly over the next year or so.
If you had lot of numbness before surgery, some feeling may return but it probably won’t go away completely.
After the surgery you may still have some neck pain.
How will I control my post-surgery pain?
We help make your stay in hospital as comfortable and pain-free as possible. Our dedicated pain team who will visit you if needed.
You may have one or a combination of drugs and methods depending on the procedure you have had. You might have some pain relief during surgery and others after you wake up.
If you have any questions or concerns about the management of your pain, ask any member of the team. There’s evidence that reducing pain and anxiety helps recovery after surgery.
During your stay in hospital, we’ll ask you to measure your pain when you move. This helps the nurse give you the most suitable pain relief to control your pain.
We use a score to measure your pain on a scale of 0 to 10. 0 is no pain and 10 is severe pain.
Recovery from day of surgery to discharge
Day of surgery |
Pre-discharge to home |
Discharge goals |
|
Nutrition and elimination |
Nil by mouth before the operation
Intravenous until you can manage oral fluids Eat light supper Sit out on the commode |
Eat and drink
Walk to the toilet Bowels opened before discharge |
Appetite returned
Passing urine with no problem |
| Hygiene | Shower/bath before the operation
Mouth care after the operation |
Help with hygiene care
Shower with help |
Fresh and comfortable |
| Wound care | Observation of incision and drainage if needed |
Check if dressing is dry and intact
If yes, no change of dressing needed |
Healing noted |
| Pain control | Intravenous analgesia (uncommon) and oral NSAIDNonsteroidal anti-inflammatory drugs, for example, ibuprofen |
Oral pain relief | Pain controlled |
| Activity and rehabilitation | As soon as you and the nurses feel you can, you can walk to the toilet with assistance.
Unless instructed otherwise |
Sit in an upright chair, dining chair or a supported chair.Sit for meals.Gradually increase sitting time for short period over a week as comfort allowsFor the first few weeks, until 6/52 post discharge, you should not do any repeated bending or any lifting |
Mobilise comfortably |
| Discharge planning | Anticipated date of discharge | Follow-up appointment organised and sentMedication TTO’s (to take out) writtenPractice nurse letter and TTO’s suppliedStocking instructionHelpful hints |
Everything explained and understood |
What exercises can I do after surgery?
After a single level ACDF or ACD-R operation you should start trying to move your neck as soon as you can. To begin with this may feel a little uncomfortable. The aim is to do small amounts of neck movement on a regular basis.
Our physiotherapists will see you while you’re in hospital and give you some simple exercises to do. The exercises will help you recover after your neck surgery.
Remember these exercises should be slow and gentle and done within a comfortable range. Never push exercise into a painful range.
You may feel some discomfort. This is normal but if your pain increases do the exercises more gently with fewer repetitions. If your pain continues, stop the exercises for a few days and gently build them back up.
Use the pictures below as a guide. We don’t expect you to necessarily reach the same range.
Ankle/quads (thighs)/glutes (buttocks)
Step 1
Bend your ankles up, then point your toes away from you. Repeat 20 times
Step 2
Circle your ankles clockwise and anticlockwise.
Step 3
Repeat 20 circles in each direction.
Step 4
Tense your upper thigh muscles. Hold for 5 seconds and repeat 5 to 10 times on each leg.
Step 5
Repeat tensing your glutes (buttocks) to hold for 5 seconds and repeat 5 to 10 times on each side.

Illustration of ankle flexing
Side bending movements
Gently tilt your head by bringing your ear towards your shoulder. Repeat on the other side.
Repeat 3 to 5 times each side.
Illustration of someone bending their head from side to side
Head turning movements
With your chin tucked in, gently turn your head to the side as far as comfortable. Repeat on the other side.
Repeat 3 to 5 times each side.

Illustration of someone turning their head from left to right
Neck bending
Bend your head down gently but not to the point of pain or stretch. Repeat 3 to 5 times.
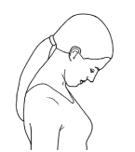
Illustration of someone bending their head down
Walking
The best exercise you can do is walking. Gradually increase the amount you do each day.
Make sure you change position regularly, around every 30 minutes, to avoid feeling stiff.
Everyone progresses at different rates post operatively. It’s important to do things slowly at first and build up the amount you do gradually. Good and bad days are normal.
What can I do to help myself recover well after surgery?
Take regular pain relief
Some pain is normal after surgery. This will lessen to a dull ache after 48 to 72 hours after the operation.
Pain control is important, particularly in the first few days and weeks. It’s best to take regular pain relief instead of letting pain build up. This will help you feel comfortable and able to get active.
Keep your wound clean and dry
Your wound like any cut may feel sore to begin with but you won’t do any damage by moving.
We’ll only change the dressing as needed. You may need to visit your GP/practice nurse for a wound check or to trim your stitches. We’ll tell you if you need to do this
Keep your wound clean and dry following surgery. Most dressings are shower proof but ask your nurse before you go home.
Don’t spend long periods lying down
You can lie in whatever position you find comfortable. It’s normal to spend short periods of time on the bed after surgery, expecially for the for the first few days. Don’t spend long periods in the day lying down.
Roll on your side to get out of bed
You may find it easier initially to:
- roll onto your side
- bend your hips and knee
- swing your legs over the side
- push up with your hands.
You can progress to getting up normally over the next few weeks.
Sit in an upright chair
You may find you’re more comfortable in an upright supportive chair instead of low chairs or sofas for the first couple of weeks.
Try using a lumbar roll or cushion in the small of your back for comfort when sitting. Change position regularly, alternating between lying, sitting and walking to avoid feeling stiff.

Illustration showing good posture

Illustration showing bad posture
Washing/bathing
Shower or strip wash for the first few weeks instead of using the bath until the wound fully heals and dried. Being comfortable getting in and out of the bath and sitting in the bath may take a few weeks.
Rest
Rest for short periods if you need to, but try to alternate rest with gentle exercise and gradually increasing to normal activity.
Go for short walks daily. Don’t spend all day lying down.
When can I restart your normal activities?
Timescales depend on your surgery. If you’ve had a fusion the timescales may take longer.
You may have had problems with balance and weakness affecting walking and arm function before your operation. It can be hard to predict expected improvement which may affect how quickly you can return to normal activities.
Lifting
Avoid heavier liftingfor the first 3 months after surgery. You can lift a lighter weight like a full kettle from about 3 weeks. You must keep your arms close to your body with your neck in a good position.
Bending forwards
Avoid excessive bending forward for the first couple of weeks. It’s easier to bend from your knees instead of your back. You may need some help initially putting on your shoes and socks. Many people get slip-on shoes or put them on in a seated position by crossing their legs over. A shoe horn may be useful.
Work
You must get fit to return to work which means gradually increasing what you do each day. You don’t need to be completely pain free to return to work.
You can return to work as soon as you feel comfortable to do so, as discussed with your surgeon.
If your work involves sitting at a desk, you can return to work after 3 to 4 weeks as long as you can keep moving.
If you have a heavy manual job you may need longer to recover (8 to 12 weeks). When returning to work, it’s likely you’ll need to gradually increase your working hours and days over a few weeks before returning full-time. This is called a phased return. Talk to your employer’s HR department or occupational health.
Driving
As a passenger, recline the passenger seat in the car slightly to make it easier to get in and out of the vehicle.
You can’t drive for at least 2 to 4 weeks. If you’ve had a fusion then may be longer.
When you’ve considered whether to drive, you must:
- have no altered sensation or weakness in your arms
- be able to move your head freely
- feel confident enough to do an emergency stop with full pressure on the brake pedal with no significant pain in your arm or neck.
Break up long journeys so you can change position and move around. Gradually increase the distance you travel, initially no longer than 20 minutes, over the next 4 to 8 weeks.
Check with your insurance company and with the Drivers Medical Group at the DVLA in Swansea. You may need to tell them that you’ve had an operation. You can get more advice at your outpatient appointment.
Sex
There’s no reason to avoid sex during the recovery period. You might prefer to be the passive partner or try different positions to find the most comfortable for you.
Activity, exercise and sport
It’s important to keep as mobile as soon as you can after surgery as this reduces your risk of getting a blood clot in your legs.
Get up and move regularly (every 20 minutes or so). Walking is the best activity to start after your surgery. Gradually build up the amount of walking you do each day. Walking outside is okay but be careful not to trip over on uneven ground.
Get into a routine so you gradually walk a bit further. You may find it helpful to use an app on your mobile phone to count your daily steps. Remember to put the phone in your pocket.
Check with your surgeon and physiotherapist when you can return to sporting activities like swimming or golf. Advice ranges from between 6 weeks to 3 months.
For previously fit sports people, you can resume training at 12 weeks, or take part in non-contact sports. All activities will need a gradual increase in time spent on the activity, activity intensity, and frequency.
You mustn’t do an any impact sports such as jumping or running for the first 12 weeks.
When will I see the surgeon’s team for a review?
A doctor will see you at an outpatient clinic around 6 weeks after the operation to check your progress. Discuss any queries you may have when you’re at the clinic.
We may need to make further outpatient appointments if necessary. For single-level ACDF or ACDR, your surgeon will request an outpatient physiotherapy appointment to start 4 weeks after your surgery.
For other types of surgery, the surgeon will decide when physiotherapy should start.
What should I do if I have any problems?
Call 01494 426398 or 111 or go to A&E out of office hours if you:
- have a high temperature of 38C or above
- have increasing pain, numbness or weakness in your legs, back or buttocks
- can’t move your legs
- can’t pee or control your bladder
- have a severe headache
- get a sudden shortness of breath (this could be a sign of pulmonary embolism, pneumonia or other heart and lung problems).
Also, if:
- your stitches come out
- your dressing gets soaked with blood
- your wound leaks fluid or there’s redness.
Links and resources
Patient information about other back and spine conditions
Causes, treatment and help for neck pain
How can I help reduce healthcare associated infections?
Infection prevention and control is important to the wellbeing of our patients so we have procedures in place. Keeping your hands clean is an effective way of preventing the spread of infections.
You, and anyone visiting you, must use the hand sanitiser available at the entrance to every ward before coming in and after you leave. You may need to wash your hands at the sink using soap and water. Hand sanitisers are not suitable for dealing with patients who have symptoms of diarrhoea.
More help or advice
Contact our patient advice and liaison service (PALS) on 01296 316042 or bht.pals@nhs.net
About our patient information
We aim to make the information as up to date and accurate as possible, but please note that it’s subject to change. You must always check specific advice on any concerns you may have with your doctor.
Contact us
01296 838888 (option 4)
01296 315050 – Ward 1
01296 316503 – Ward 2
01494 426398 – Ward 12B
01494 734109 – Amersham Hospital
01494 425431 – Wycombe Hospital
01296 315087 – Stoke Mandeville
