Investigation of your gut: an endoscopic retrograde cholangio pancreatogram (ERCP)
Read our guide below to understand what to expect from a endoscopic retrograde cholangio pancreatogram.
You can also download a PDF version of this patient information by following the link on the right.
You’ve been advised by your doctor to have an investigation known as an ERCP.
Your appointment
If the time or date isn’t convenient, call the Endoscopy department as soon as possible on 01296 831210. We can reschedule your appointment.
What is an ERCP?
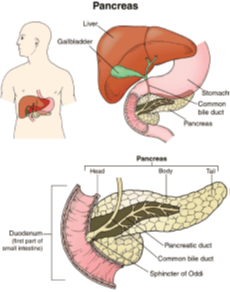
It’s a procedure which combines the use of an endoscope (a flexible telescope to look inside your gut) and x-rays. It’s used mainly to diagnose conditions that affect the bile ducts and pancreas. It’s often possible to treat the condition at the same time.
The endoscope is passed down through the stomach to find the exit of the bile duct and pancreas.
A small tube is then passed through the endoscope into this opening, and dye which shows up under x-ray is injected. This enables the endoscopist to decide whether any disease is present and, if so, treatment can take place through the endoscope at the same time.
If the x-rays show a gallstone, the endoscopist may enlarge the opening of the bile duct by making a very small incision with an electrically heated wire (diathermy), which you won’t feel.
The gallstones will be collected in a tiny basket or left to pass into the intestine.
If a narrowing is found preventing the passage of bile a short tube (stent) can be placed in the bile duct. You will not be aware of the presence of the tube, which can remain in place permanently. Occasionally, it may be necessary to replace the tube.
Consent
All procedures done in hospital need your consent. This is a legal requirement.
Read this information carefully. It will help you to make an informed choice, and help you understand the risks associated with your procedure.
Admission to hospital
During the admission stage, one of the endoscopy specialist nurses will explain your procedure and go through the risks associated. You’ll have the opportunity to ask questions. Once you’re completely happy, we’ll ask you to sign a consent form. Please note you have the right to withdraw your consent at any time.
What happens to my written consent?
Your signed consent is held in our hospital notes. If you want a copy, we can organise one for your personal records.
Tissue samples
For some procedures, we take tissue samples for microscopic examination. Instead of destroying the samples after this examination, we ask your permission to use these tissue samples for teaching and research purposes. We treat all specimens anonymously.
If you need a translator
If you don’t speak English, an independent translator should be available to make sure you understand the test. We prefer this to a member of your family or friend translating for you.
If we can’t get proper consent, we’ll cancel the procedure.
What does the procedure involve?
Before you enter the endoscopy room, you’ll have a rectal suppository (a medication given through your anus). This is to reduce the risk of pancreatitis (inflammation of your pancreas). You may also be given fluids through a cannula tube in your vein.
In the endoscopy room you’ll be made comfortable on a trolley and asked to lie on your left side. A nurse will stay with you throughout the test. The procedure is done by a trained doctor or nurse called an endoscopist. We’ll ask you to remove your glasses and dentures.
Remove jewellery or metallic objects as they interfere with x-rays and diathermy (a treatment using high frequency electricity).
A plastic mouthpiece will be placed gently between your teeth or gums, to keep your mouth open. The endoscopist will pass the endoscope through the mouthpiece and gently down. It shouldn’t cause any pain or interfere with your breathing at any time.
During the test some air will pass down the endoscope to distend the stomach. This is done to give the endoscopist a clear view and may cause some temporary discomfort. When the examination is finished, the endoscope is removed quickly and easily and the air is sucked out.
For your comfort, you will be advised to have sedation and throat spray.
Sedation is given to you through an intravenous cannula (a small plastic tube put into your vein). It’s a sedative not an anaesthetic and will make most people
feel drowsy and relaxed.
Throat spray will numb the back of your throat and help to make it less sensitive.
Are there any risks involved?
An ERCP is a skilled procedure and is performed by a highly trained endoscopist who takes every care to reduce any risks.
The main risk linked to ERCP is inflammation of the pancreas (pancreatitis). The risk of this occurring is 5% (1 in 20 patients) and the risk of death is 0.3% (1 in 300).
If special treatment is needed during the procedure to help remove a gallstone, for example, an incision will be made in the lower end of your bile duct (sphincterotomy). There’s a slight chance of bleeding or perforation from this incision (about 2% of patients). These problems usually settle down on their own, though they may delay your return home by a few days.
Very rarely, an operation is necessary to treat a complication.
Mechanical damage to teeth or bridgework
We’ll ask you to remove any dentures and insert a mouth guard before the procedure. This will protect your teeth and reduce the risk of you biting the scope.
Risk of a missed lesion
Although this has been chosen as the best test to diagnose your symptoms, no test is perfect. There’s a risk of 1 in a 100 that we might miss a lesion or other important finding during your test.
Risks associated with having sedation
Sedation may occasionally cause problems with slower breathing, low blood pressure and a slow heart rate. Careful monitoring of these vital signs during the procedure will detect any changes early so that we can treat these quickly.
What do I need to do before my appointment?
You’ll need to take some time off work and may need to stay in hospital for 2 to 4 hours. The unit closes at 6pm. Appointment times aren’t exact as the unit sometimes needs to respond to unexpected emergencies so occasional delays are inevitable.
We’ll discuss the results with you before you leave.
If you’re asthmatic, bring your inhalers with you and let the nurse know.
If you have diabetes, tell the clerk when booking your appointment. Bring your diabetes tablets or insulin with you on the day. If you need advice about controlling your blood sugars before and after the procedure, contact your Diabetes Nurse Specialist or GP.
If you have sleep apnoea, tell the nurse as you may not be able to have sedation for the test.
If you’re taking Warfarin or any other blood thinning tablets, tell the Endoscopy booking clerk or pre-assessment nurse when making your appointment.
Other blood thinning tablets include:
- Rivoroxaban
- Dabigatran
- Apixaban
- Edoxaban
- Clopidogrel
- other ‘antiplatelet’ drugs.
You can continue taking Aspirin.
Is there anything else I need to bring?
Yes. Please bring a list of your medication with you.
Do not bring any valuable items or jewellery.
Preparation for your appointment
If your appointment’s in the morning:
- do not have anything to eat or drink from midnight of the night before the examination. Food or liquids will obscure the view of the endoscope and the examination will not be possible.
- you can have a small glass of water no later than 2 hours before your appointment time
bring your regular medication with you and you can take it after your procedure.
If your appointment’s in the afternoon:
- have a light breakfast before 8am. We recommend toast and tea. Do not eat porridge or eggs
- have your last drink at least 4 hours before your appointment. Avoid milky drinks
- have a small glass of water no later than 2 hours before your appointment time
- if you take regular medication in the morning, take it as usual.
What happens when I arrive?
The receptionist will book you in and a member of the Endoscopy nursing team will collect you from the reception area. If you haven’t already been seen for a pre-assessment discussion, we’ll take you to a private room to get a brief medical history.
The nurse will explain the risks involved in the procedure. You’ll have the opportunity to ask questions. You can also sign your consent form if you haven’t already done so.
Family friends and relatives
After the pre-assessment, we’ll ask anyone accompanying you to return to the reception area until after your procedure.
Refreshment facilities are available at:
- Stoke Mandeville Hospital. There’s a restaurant in the main entrance (entrance 3)
- Wycombe Hospital. There’s a café within reception at main entrance (ground floor of the main tower block)
- A doctor or one of the endoscopy nurses will discuss the results of your test with you before your discharge from hospital.
What are the possible side effects of the procedure?
You’re likely to have a sore throat after the procedure. You may also feel bloated from the air blown in to help the examination.
It’s not uncommon to experience some discomfort immediately following the procedure due to air in the stomach. This is usually mild and will soon pass with the help of warm drinks, walking around, drinking peppermint water or eating sweets.
Very rarely, more severe abdominal pain, sickness or a temperature may happen due to an inflammation of the pancreas (pancreatitis). This might require a few days’ stay in hospital for pain relief and antibiotics until it settles.
What are the after-effects of the sedative injection?
Your mental ability to think clearly and make decisions may be affected for up to 24 hours after the procedure, even though you feel wide-awake.
For this reason, you must have someone who can take you home and look after you for the rest of the day. You may resume eating as normal.
For 8 hours after sedation, you must not:
- use potentially dangerous appliances such as a cooker or kettle
- have a bath unsupervised
- look after dependants on your own
- go to work
- sign any legal documents
- drink alcohol
- take sleeping tablets or recreational drugs.
For 24 hours after sedation, you should not:
- drive
- operate potentially dangerous machinery.
Starting to eat again
You should avoid large or rich meals for the rest of the day following your procedure.
Medications
You may resume normal medications immediately after your ERCP. Ask if you’re not sure if it’s safe to take your medication with the sedation.
Advice
Call us if you’re worried about any symptoms you have after this test.
How to get help after the test
If you have any severe chest or abdominal pain, particularly on swallowing, or if you vomit blood, get help immediately.
During normal office hours
Stoke Mandeville Hospital, 01296 315220
Wycombe Hospital, 01494 425073
Outside office hours
Call Ward 17 at Stoke Mandeville Hospital on 01296 418201.
This is for patients who had their procedure in Wycombe or Stoke Mandeville hospitals.
In an emergency, come directly to Stoke Mandeville Hospital Emergency Department
Follow up information
You’ll need to:
- see your GP for treatment. Take the copy of the report with you to your GP appointment
- have an appointment in our outpatients clinic
- have another investigation
- talk to your GP and/or consultant about your biopsy results in approximately 8 weeks. We’ll contact you if further action is necessary.
Useful links
Buckinghamshire Healthcare NHS Trust
British Society of Gastroenterology
Guts UK Digestive Disorders Information
