Speech and language difficulties we work with
We see children and young people with a range of speech and language challenges and specialise in specific areas.
Find out more about our the communication difficulty your child may have and what you can expect.
What is Developmental Language Disorder?
Some children have difficulties learning and using language, that are not associated with other factors (such as autistic spectrum conditions, hearing impairment, other sensory impairments or more general learning difficulties, although these conditions may co-occur). The language difficulties are also not due to the child learning English as an additional language.
Language disorder refers to children’s language difficulties that impact on communication and or/learning in everyday life, and where past research indicates they are unlikely to catch up spontaneously. If the language disorder is associated with another known condition it is referred to as “Language Disorder associated with X”, where X is the known condition. A child may have a Language Disorder associated with autistic spectrum disorder, for example.
Those children who have more persistent difficulties with language than other areas of learning and development, which are not likely to resolve by 5 years of age, and which are not associated with another condition, can be described as having Developmental Language Disorder (DLD). These children may also develop communication skills in a different way to other children. These children may not make the expected progress despite targeted intervention.
DLD can be hard to understand as there is no known cause. It is not caused by emotional difficulties or by parents not talking enough to their children. Children with DLD can have co-occurring difficulties such as dyslexia, ADHD and speech sound difficulties. On average around two children in every classroom have DLD, but it can be hard to spot. It is therefore often described as the “hidden” disability. DLD affects and impacts on different children in different ways. Some of the things that children with DLD might find difficult include:
- Following or remembering spoken instructions.
- Organising ideas so that they are able to verbally express what they want to say.
- Telling or re-telling a coherent story
- Finding the right words (vocabulary) to say at the right times
- Understanding what is read or listened to.
- Over-literal interpretation, missing the point of what was meant.
- Talking a lot but engaging poorly in two-way conversation.
What is DLD?
Watch the video below about DLD and what every teachers needs to know:
Please look out for live webinars that are run throughout the academic year. Others may find this a valuable way to access deeper understanding of DLD.
What is the impact of DLD?
DLD can affect all areas of life: including learning, communicating, developing literacy skills, making and keeping friends and having a healthy mental and emotional well-being. Children with DLD may find it difficult to achieve academic success at school. Sometimes children withdraw and become passive. Sometimes difficulties and anxieties linked to DLD can be wrongly interpreted as misbehaviour. DLD is a long-term condition and difficulties can persist into and throughout adulthood.
Want to find out more about DLD?
On the NAPLIC website you can find a collection of regularly updated articles relating to DLD.
Language Difficulties/Speech, Language and Communication Needs in the Early Years
It can be difficult to predict Developmental Language Disorder in young children, and it becomes easier to identify if difficulties persist beyond 5 years of age. Children can also need support in other areas (e.g. social skills, speech difficulties) which are secondary to their language needs.
What might I notice if a pre-school child has Speech, Language and Communication Needs that may persist into the school-aged years?
There may be a family history of language and or/literacy difficulties.
And these are the Early Years Red Flags for atypical language development set out by researchers for all to be mindful of and to monitor:
1-2 years:
- No babbling
- Not responsive to speech and/or sound.
- Late talkers with poor understanding of language
- Minimal or no communication attempts.
- Poor use of gesture, e.g. fewer than 16 gestures at 16 months.
2-3 years:
- Minimal interaction
- No intent
- No/few words – not putting two words together
- Minimal reaction to spoken language
- Regression or stalling of language development
3-4 years:
- inconsistent or abnormal interactions
- 2-3 word utterances at most
- Difficulties understanding simple instructions
- Difficulties understanding and using verbs
- Close relatives cannot understand much of what the child says
4-5 years:
- May not be able to repeat nonsense words
- May have words and be talking in sentences, however strangers cannot understand much of what the child says and close relatives cannot understand more than half, even in the absence of speech sound difficulties.
NOTE: It is important to note that not all children with these atypical features of language development will go on to receive a diagnosis of DLD. Some children’s difficulties may resolve spontaneously. Other children may go on to receive another diagnosis, e.g. Language Disorder Associated with… (another known condition).
However, the more severe the difficulties are, and the more areas of language development affected, the more likely they are to persist.
Advice for Settings
Children may be identified as having a Developmental Language Disorder in the Primary or Secondary Phases of Education. The Buckinghamshire Speech and Language Therapy Service provides support at all key stages and for some students this may continue into Further Education Settings.
Here is a more comprehensive list of key indicators or “red flags” that may be seen in junior and secondary aged young people:
- Difficulties with following instructions, particularly if they are long or contain complex vocabulary
- Difficulties with understanding and answering questions, including more complex forms e.g. why? How?
- Difficulties with remembering, recalling and understanding vocabulary and using words in the correct context
- Struggling to construct spoken and written sentences accurately with correct grammar and meaning. They might use shorter sentences than peers and produce sentences with errors in tense and pronouns.
- Difficulties with understanding and generating narrative, including sequencing
- Difficulties using language in social situations e.g. understanding unwritten rules of conversation, understanding non-literal language, idioms and inferencing
- Word finding difficulties
- Difficulties understanding concepts – especially Maths and Science words that relate to time, size, comparison and measures.
Watch an extremely helpful training video, “Developmental Language Disorder (DLD) – What every class teacher needs to know”. This video has been especially created for education staff by Moor House School, a specialist setting for children with DLD.
DLD Additionally Resourced Provisions
Some mainstream schools in Buckinghamshire have an Additionally Resourced Provision (ARP), which is a specialist placement for children with DLD. Children who attend an ARP benefit from intensive and flexible Speech and Language Therapy and Specialist Teaching on site, according to their needs. They are members of mainstream classes and are taught alongside their peers within the classroom, receiving some teaching by experienced teaching staff. At times, children may receive specialist small group teaching as part of their ARP provision.
Videos that Support Understanding of DLD and the Needs of a Child or Young Adult with DLD:
- DLD The Consensus Explained – Professor Dorothy Bishop explains how consensus was achieved and the term “Developmental Language Disorder” was agreed upon.
- Lily Farrington – In this enlightening video we meet Lily Farrington, who was diagnosed with DLD at 15 years of age. Lily explains what it is like to have Developmental Language Disorder.
- This is Me and DLD – In this video produced in Dorset, a young child talks about his difficulties as a child with DLD and how it makes him feel like an alien.
- Supporting Developmental Language Disorders in the Classroom – This American YouTube production explains clearly the impact of DLD in the classroom and how understanding the difficulties associated with DLD is critical so that a child with DLD is correctly supported.
- #ThinkLanguage #ThinkDLD – This excellent video was produced for a past DLD Awareness Day and again focuses on the impact of DLD in the classroom.
A “DLD Awareness Day” is held each October. The RADLD website constantly produces more and more information, top tips and support information about DLD so revisit regularly.
What is it?
A Cleft lip or palate is formed when parts of a baby’s face did not join together properly during development in the womb. Some children can have a cleft lip (a split in their upper lip), a cleft palate (a split in the roof of the mouth) or both.
In some cases, a child may have a submucous cleft palate. This is where the split or cleft occurs only in the soft palate at the back of the mouth. As this is covered by the lining of the mouth it may not be noticed at birth, often being diagnosed only when symptoms develop (such as difficulties feeding/swallowing or producing certain speech sounds).
Support
The Speech and Language therapy service works with the regional cleft lip & palate centres that border Buckinghamshire. Most of the children living in Buckinghamshire are cared for by the Children’s Cleft Palate and Craniofacial service, which is based in the John Radcliffe hospital, also known as the Spires Cleft Centre. However, some children are cared for by the North Thames Cleft, or the South Thames Cleft service.
These regional services provide specialist information, assessment and therapy for children and young people with cleft lip and palate and/or velopharyngeal dysfunction, from birth into adulthood. This is delivered within the context of the multi-disciplinary Cleft Team and in partnership with families, settings and local Speech and Language Therapy services across the region. Our Buckinghamshire speech & language therapy service has therapists who work locally to support the work of the cleft centres.
Find out more:
For more information visit:
- Cleft lip and palate (NHS)
- The Spires Cleft Lip & Palate Centre
- North Thames cleft lip & palate centre
- South Thames Cleft Service (St Evelina’s)
- Cleft Lip and Palate Association
What are they?
They’re a result of conditions including:
- cerebral palsy
- genetic conditions
- severe epilepsy
- muscular dystrophy
- acquired brain injury, for example, head injuries including road traffic accidents and degenerative neurological conditions.
How we help early years children with complex communication needs
We support children’s communication development using spoken language, signing, symbols, and a range of other communication methods.
We assess and support children in early years settings and their homes.
Who we work with
Our therapists work with children aged from birth to 5 years with complex medical needs including:
- physical/motor impairment
- visual impairment
- neurological impairment, for example, epilepsy
- degenerative medical conditions
- chronic health needs
- acquired disorders following head injury or stroke
- social communication difficulties or autistic spectrum conditions
We also work with children who have:
- learning difficulties/global delay, including profound and multiple learning difficulties
- genetic diseases such as tuberous sclerosis
- significant additional or alternative communication needs and use a communication book/ switches/ communication aids.
How we help school aged children with complex communication needs
We assess and support children in mainstream schools, special schools and specialist settings known as additionally resourced provision (ARPs). We help children with physical disabilities to develop functional communication within the context of their needs.
We help develop the child or young person’s communication skills and access to the curriculum through:
- spoken language
- signing
- symbols
- visual timetables
- topic boards
- ICT (where appropriate).
We assess the child/young person’s suitability to use ICT to access the curriculum. We do this in collaboration with Bucks Learning Trust Specialist Teaching Service
We also support children and young people who find communicating verbally difficult by identifying augmentative, alternative communication systems (AAC). We personalise these for each individual’s current needs.
Who we work with
We work with children and young people from 5 years to 25 years with complex medical needs (see who we work with for early years above).
For both early years and school settings, we work within a multi disciplinary team including:
- class teachers
- support assistants
- occupational therapists
- physiotherapists
- paediatricians
- dieticians
- specialist teachers
- other professionals that may be involved with your child’s needs.
We also work alongside other members of our own service for example therapists specialising in hearing impairments.
How to access our teams for complex communication needs
Contact Theresa Drake, Highly Specialist Speech and Language Therapist, Clinical Team Lead at buc-tr.cyptherapies@nhs.net.
Who we work with
We work with children with different types levels and causes of Deafness of including:
- congenital (present at birth, sometimes as a result of a virus)
- acquired sensorineural (develops later in life sometimes due to aging, sudden trauma or malformation of the inner ear)
- permanent conductive (caused by a blockage of the ear canal)
- auditory neuropathy/dys-synchrony (unknown cause but children with a family history of the condition or who were born prematurely may be at higher risk).
We also work with hearing children of Deaf parents who use British Sign Language (BSL) as their home language.
Our team has experience of children who use cochlear implants, hearing aids and bone conduction aids to give them access to sound. The children we see often have a range of difficulties in addition to their hearing impairment.
If the child gets support from a different team within our service, we give advice about any needs they have which are related to their Deafness.
Watch the video below about a parent’s experience of a child with hearing loss:
What we do
We assess and support children and young people in their homes, early years settings, schools and Further Education (FE) colleges. We help them to develop effective communication within the context of their Deafness.
We use a range of communication approaches including spoken language, sign supported English, and/or BSL as appropriate.
Family support
We support families through regular visits, joint working with other professionals and groups such as ‘Little Ones’ group.
We encourage families to access local support, for example through Young Deaf Activities (YDA) and the National Deaf Children’s Society (NDCS). These organisations offer information and opportunities to meet other families and share experiences and ideas.
School and education support
We work with hearing support teachers from the Specialist Teaching Service, audiologists and specialist teams at Cochlear Implant Centres.
We see children and parents at home, and visit staff in mainstream preschools and schools. We also support in additionally resourced provisions (ARPs).
Staff can also benefit from our training sessions on working with hearing impaired children in a variety of educational settings.
How to access our team for advice and support
Contact Sarah Adams at sarah.adams4@nhs.net
We work with colleagues who have specialist clinical knowledge and experience in the difficulties associated with Down’s syndrome. These include:
- hearing impairment
- eating and drinking difficulties
- visual impairment.
How we support children with Down’s syndrome
We help by:
- developing the child’s communication environment and promoting the use of visual cues such as pictures, symbols and signing
- training parents, carers and setting staff in the use of Makaton signing
- assessing the child’s speech, language and communication needs
- providing advice and specific communication targets
- using the child’s individual learning profile and areas of strength to develop their communication skills.
Schools and education settings
We also work in the child’s school or education setting alongside staff on specific areas of communication including:
- speech production
- auditory memory
- vocabulary
- spoken sentence structures.
Our therapists work alongside the Specialist Teaching Service for children with Down’s syndrome.
What signs should I look out for?
Also known as ‘dysphagia‘, your child may have problems with chewing and swallowing certain foods and drinks. They may also show difficulties including:
- problems with oro-motor movements of eating, for example biting, sucking and chewing
- frequent chest infections
- coughing and choking whilst eating or drinking
- ‘gulpy’ swallowing actions
- watering eyes
- indifference to eating or drinking
- failure to thrive.
How we support children with eating, drinking and swallowing problems
Our team work closely with other professionals such as dieticians, health visitors, and child and adolescent mental health services (CAMHS).
We:
- assess eating and drinking skills and make judgements about swallowing safety
- suggest appropriate textures and consistencies of food and drink to support safe eating and drinking
- develop oro-motor skills to aid chewing
- provide advice and strategies, including referring onwards if appropriate.
How can I get a referral for my child?
If you’re concerned about any of the above signs, please contact your GP or consultant to get a referral. We can only accept referrals from medical professionals for this area of difficulty.
What is it?
It’s an umbrella term for the difficulties experienced by children with:
- language disorder
- Developmental Language Disorder (DLD)
- problems acquiring language and communication skills.
Monitoring your child’s development
Children develop language skills at very different rates and abilities can vary significantly in the early years. Many young children who have a limited vocabulary at 18 to 24 months will catch up with their peers over time.
Unless there are specific risk factors for DLD, or the child has language difficulties alongside another condition, research suggests monitoring your child at age 2 to 3 years.
Previous research indicates that about 40% of children identified with problems acquiring language by 4 years of age spontaneously resolve by school entry.
Difficulties may be more short-term than persistent.
School age children
At school age, we use the term LCN to describe difficulties experienced by children who do not have language disorder (associated with another biomedical condition) or DLD (severe persisting difficulties).
A child with LCN may have some language difficulties which they need help with so they can thrive in an educational setting. Schools in Buckinghamshire screen for these difficulties and resolve many of them through quality first teaching and targeted support. They may approach us for additional guidance.
How to support a child with LCN needs
See our resources to help your child develop at each stage of communication development.
You’ll find age milestones, what to expect and a range of activities to help support your child in that area.
What is it?
Also known as ‘situational mutism’, it’s a condition where children can talk comfortably in some situations, for example at home, but not others (such as playgroup, preschool or school).
Selective mutism is a form of anxiety disorder which can be thought of as akin to a phobia of speaking in specific situations.
Selective Mutism usually starts at around the age of 3-5 when a child first starts school. It is important to note that children are not “choosing” not to speak – they are unable to.
How can I tell if a child has selective mutism?
The child will consistently speak less freely in some environments.
The situations where they are unable to speak may vary with the location, type or number of people around, or type of talking.
Some children may appear ‘frozen’ in some social settings and can’t join in. Other children may seem happy to communicate non-verbally, for example, through pointing, gestures or facial expressions, but will not talk.
When the child feels comfortable, such as at home, they will be able to speak freely and confidently.
How we help children with selective mutism
The priority is to help children speak to those in the day to day environment, so we support children by training those around them. The most important thing is to first change the environment to ensure everyone knows about SM, there is no pressure on the child to speak, people talk openly about speech anxiety, and work on building the child’s confidence more broadly.
We offer guidance and initial training for settings with no referral necessary. Where concerns persist following this, children can be referred to us through the school advice clinic. We can also offer bespoke meetings to review targets and troubleshoot.
We also offer group sessions for older children over the holidays. This provides a valuable opportunity for young people with SM to meet others in the same situation, and to learn more about their condition.
How you can help
The first step will be to download our Settings Pack which contains initial guidance. Please ensure you have the correct version – these are updated annually. You should then attend our webinar. The settings packs contains the handouts you need for this webinar.
For some children (particularly those under the age of 5) following the advice given in the above webinar consistently for a term or two is usually sufficient and the Selective Mutism is likely to resolve without further input.
However, some children will need more support such as a formal Small Steps programme. How to know where this is the case will be covered during the first webinar. School staff should book onto a school advice session to discuss any continuing concerns with a speech and language therapist. Equivalent sessions are also available for early years children.
At these sessions, a referral will be made to the SM team where appropriate. NB a Language Link assessment should also be carried out prior to this school advice session.
Useful resources
How selective mutism is supported in Bucks
Find out more about selective mutism in an illustrated guide book
Get advice, support and access additional resources
Please download our Settings Pack – or email us for a copy: bht.selectivemutism@nhs.net
Watch our video below to understand more about selective mutism:
Who we work with:
We work with young people from nursery age through to further education (FE) who present with social communication difficulties or with a diagnosis of autism.
Autism is a lifelong, developmental disability which affects how people communicate and interact with the world.
You can read more about autism from the National Autistic Society (NAS) here: What is autism?
You can also view 12 fast facts about Autism below:
Or watch What is Autism? – an introduction to autism:
The Spectrum Magazine, produced by the National Autistic Society, is one of the UK’s largest collections of autistic art, poetry and prose. It provides a great insight into the experiences of autistic adults and young people: The Spectrum magazine (autism.org.uk)
The Buckinghamshire speech and language therapy service work with young people who communicate using:
- Behaviour (e.g. pulling and leading by the hand)
- Vocalisations (sounds which might not be clear words)
- Gestures (e.g. putting their hand up to communicate ‘stop’)
- Pictures (this may be through paper resources or high-tech devices)
- Sign language (such as Makaton)
- Ecolalia (e.g. repeating words or whole phrases)
- Speech (single words through to complex sentences)
We carry out our work within a total communication approach – all methods of communication are valid and we will work hard to find the type of communication that is most accessible to the young person you are supporting.
What we do
We assess and support children and young people in their homes, early years settings, schools and Further Education (FE) colleges. We help them to develop effective communication within the context of their communication differences and neurodivergence.
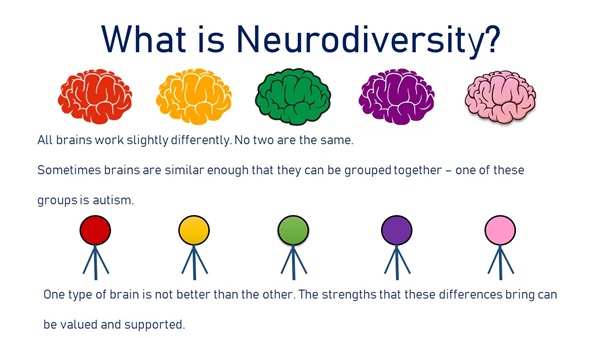
Neurodiversity refers to difference in our brains, see the infographic below for more information.
Here a specialist teacher talks us through what neurodiversity is and how we can adapt education to suit a wide range of students.
Neurodiversity in education (autism.org.uk)
The young people we work with may need support to engage, interact and communicate with others. We work with the individual on these areas through child-led, meaningful activities which are motivating and relevant to the young person’s priorities.
Family support
We support families/ carers to understand their child’s communication skills and preferences. This is delivered through the coaching of adults in how to engage with their child in a way that fosters mutual enjoyment and connection.
We encourage families to access local support through the Early Bird program and the NAS (National Autistic Society). These organisations offer information and opportunities to meet other families and share experiences and ideas.
School and education support
We work with teachers and education staff, Paediatricians, Educational Psychology, Specialist Teaching Service, Occupational Therapy and CAMHS to provide a team around the child/ young person.
We see young people and parents/carers at home and visit staff in mainstream preschools and schools. We also support in additionally resourced provisions (ARPs).
Our work involves
- supporting educational settings in adapting the learning environment
- developing the knowledge, confidence and skills of education staff working with young people
- providing therapy for specific speech, language or communication needs occurring alongside social communication needs/autism
- training early years and school staff. Please use the following link to see the training opportunities we offer: Training for parents, early years and school staff – Buckinghamshire Healthcare NHS Trust – CYP Website (buckshealthcare.nhs.uk)
This work is carried out within the context of a neurodiversity affirming framework.
How to access our team for advice and support
Please visit our resource pages or to speak to a speech and language therapist to request a virtual advice session
What are Speech Sound Disorders?
Speech Sound Disorders is a term used to describe the difficulties that some children have with pronunciation. It covers difficulties with making the right speech sound (articulation), using sounds in words (phonology) as well as using the right rhythm and emphasis/stress on words in conversation.
A variety of other terms are also used to describe Speech Sound Disorders including speech delay and speech disorder, and in some cases, dyspraxia.
How can I tell if a child might have a Speech Sound Disorder?
Children typically vary in their speech development. Younger children produce speech which is different to adult speech. So, a child’s speech development may be within the normal range, depending on their age and which sounds they are having problems with. However there are children who may be having more difficulties with learning to make the right movements to say specific sounds, or having difficulties making sounds into words.
There are variations in how adults produce speech as well, so the ‘errors’ which some children make in their speech might be more accurately described as a speech difference, rather than a speech difficulty. We need to think about the impact of any speech difference on how well children are understood and acceptability of the child’s speech to others.
You may notice that your child:
- is talking, but is very difficult to understand
- has only a few consonant speech sounds compared with what might be expected for their age e.g. they may only be using “d” or “g” sounds
- misses out lots of sounds or parts of words (syllables) when they talk
- doesn’t say the right vowel sounds e.g. says “bad” instead of “bed”
- seems to be easier to understand when they say single words but is much harder to understand when they talk in phrases or sentences.
- can copy lots of individual speech sounds, but can’t say them in words
Take a look at our Speech and sound awareness section to get more information about speech sound development.
How we help children with Speech Sound Disorders?
Speech and language therapy aims to identify whether the child’s speech is not within the typical range expected for the child’s age, diagnose the type of speech sound disorder, decide with the parent whether the child would benefit from intervention, and provide appropriate intervention.
Some children have difference in speech development that resolve with advice and maturity.
If your child has not yet started school, then we offer support and information through the parent and carer advice sessions for early years speech and language therapy virtual advice sessions. This may be the only speech therapy support that some children will need. However, if speech does not develop as anticipated following advice, or if there are signs of unusual or restricted speech development then your child might be offered a screening assessment.
If your child is at school, then your child’s school can use the SpeechLink resources to assess and treat a wide range of speech sound difficulties. Schools can also seek advice and support from the School Advice Clinic to compliment the SpeechLink support or request additional help. A referral to the Speech Sound Disorders team may also be discussed. You can also take a look at our speech and language therapy virtual advice sessions.
If your child does have a speech assessment from the speech & language therapist and is found to have speech sound disorder, then we know that more complex or persisting speech disorders do best when supported by parents, nursery/school staff and speech & language therapists. We have a team of therapists providing therapy from our health clinics for children with these types of speech sound disorder. This team is called the Speech Sound Disorders team.
How you can help
All children can be supported with speech sound development.
You can help by carrying out any activities recommended either in the advice session, via your child’s school from the SpeechLink programme, or any parent programmes sent home by your child’s school.
What is stammering?
Also known as stuttering or ‘dysfluency’, stammering is when someone:
- repeats sounds or syllables, for example, saying “mu-mu-mu-mummy”
- make sounds longer – for example, “mmmmmmummy”
- gets stuck on a word or it does not come out at all.
It’s a complex difficulty that can vary at different ages, in different situations and for different children. It is relatively common for children under 5 years old years old to go through a short phase of stammering, especially when they feel under pressure to communicate.
Early intervention
It’s less likely that older children who stammer go through a short-term stage. Early intervention is beneficial for children who stammer. We advise you to refer a child who stammers for more than a couple of months, or if you’re concerned.
How we help children who stammer – what to expect
Assessment
When you bring your child to us for the first time, we’ll discuss your concerns find out a little about your child’s medical and developmental background. We may check language development and, for older children, talk to them about their feelings about their speech.
We will then discuss the next steps with you, including what you can do to help which. For younger children this will include special time.
Telephone monitoring (for children under 7)
Research shows that young children under 5 can stammer for a few weeks or months and then stop without needing any therapy. Research also suggests there’s no risk in waiting 12 months after a child has begun to stammer before beginning therapy.
We offer a telephone review service for young children to check their progress. We’ll discuss how you are getting on with special time and ask if your child’s speech has changed.
If we can not call you, we’ll ask you to complete a questionnaire. More than half of the children who come to our clinics with a stammer never need therapy.
Individual therapy
If we recommend therapy, we’ll call you to arrange an appointment with you and your child. We usually offer children under the age of 7 Lidcombe therapy or Parent-Child Interaction therapy.
We’ll explain these to you fully when therapy begins. Both approaches involve lots of play and need a commitment from parents to attend therapy sessions and work with their child at home.
Block therapy sessions
We may offer children aged 7 years and older a block of 6 individual therapy sessions. Therapy for older children is more direct. We help them to change the way they speak by teaching them speech techniques, but also work on their communication and confidence.
Parents attend these sessions and will need to help with home practice.
We may offer Skype sessions to some older children. You can discuss this with your therapist.
Group therapy
We offer 3 different groups depending on a child’s age:
- Smoothies for children aged 7 to 9 years
- Blockbusters for children aged 10 to 12 years
- Teen Challenge for children aged 13 to 15 years.
We help improve communication and confidence as well as helping with speech techniques. Parents do not attend these sessions but we expect them to help with home practice.
The Smoothie and Blockbuster groups take place during school hours. Each group lasts 5 weeks with Smoothie sessions lasting 1 hour and Blockbusters 1.5 hours. We then follow up a few months later.
The Teenage group usually takes place during half-term and holidays. We usually run 2 sessions during each holiday break (excluding Christmas).
Stammering in older children is relatively uncommon so we do not run groups throughout the year. You may need to travel for our group sessions but we try to place children in suitable locations.
I’m a teacher. How can I support a child who stammers?
Get advice and resources on how you can support children who stammer. Or email bht.stammering@nhs.net to attend out termly training for teaching staff.
I’m a parent, carer or young person who stammers. Where can I get further advice and support?
Voice refers to the way we produce sounds for talking using our lungs and vocal cords (or vocal folds).
How we can help
We give advice to help children and young people look after their voices. Disorders of the voice involve problems with volume and quality.
