Totally implanted central venous access device (portacath)
You have been advised that the most effective way for you to get your treatment is through a totally implanted venous access device called a portacath or port.
What is a port?
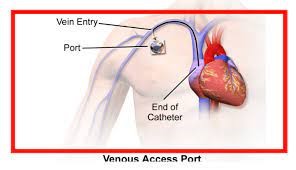
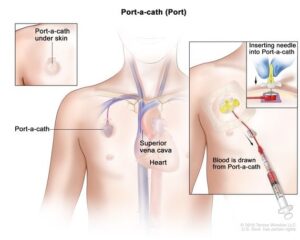
The port is a hard plastic round shaped device with a silicone gel in the centre. This device is placed under the skin, in a pocket of tissue which is usually on the chest or in your arm.
Attached to the port is a soft, hollow tube which is inserted into a large vein which leads into the blood stream around your heart.
The port can give you fluids, blood products and medicines, and we can use it to take blood samples. It’s designed to stay in your body for many months or even years.
What does the port include?
It’s made up of:
- the portal – a small chamber with a self-sealing silicone where we insert a special needle
- the catheter made from a soft, non-irritant material that the medication is administered through.
- a connector which joins the portal and catheter together.
How is the port inserted?
A healthcare professional will do this in the radiology department using a local anaesthetic or sedation
Possible risks and complications
Every procedure has some risks and complications. Your healthcare professional will explain these to you before they insert the port. They’ll ask you to agree and get your consent to go ahead.
After the procedure, tell your nurse or doctor if you have:
- fresh bleeding or discharge at the point of entry
- swelling, redness or pain that spreads on your chest or arm
- a temperature or feel feverish.
Using your port
Your nurse or clinician will insert a special needle, known as a huber needle through the skin into the silicone section of the port.
You can have a skin anaesthetic to help numb the area if you need it before the needle insertion. Over time the skin over the port often becomes de-sensatised.
Once the needle is in position, we will put a dressing over the top to hold it in place and help protect it from infection and keeps it dry.
You’ll get more specific instructions depending on your treatment needs.
Caring for your port?
Once a needle has been inserted into the port, the needle can remain in place for 7 days, before it needs changing.
Depending on your treatment, a nurse or healthcare professional will flush the port with sodium chloride (saline) through the needle extension set. Administer your treatment and then flush the needle extension again with sodium chloride and a heparin/saline mix to help stop any blockage to the catheter tip.
They will either remove the needle if you are not due any further treatment or leave it in place until your cycle of treatment is complete or at 7 days
It is recommended that you have the port flushed and accessed every 4 to 6 weeks if you’re not using it for treatment. The unit/specialist team looking after you will discuss this with you and make these arrangements.
Baths and showers
The dressing that was put on when the port was accessed with a needle is waterproof and suitable to remain for showering. Try not to soak the dressing under the shower.
Remove any excess water from the dressing by dabbing it dry.
You can swim when your port is not accessed with a needle and the site is free from infection. Always talk to the team looking after you about any concerns.
How is the port removed?
A healthcare professional in the radiology department will remove the port if you have any complications or when your doctor decides you no longer need it.
You’ll have a local anaesthetic and an incision in the skin to remove the port as well as the catheter tube.
You’ll have steristrips or stitches in place, which we’ll discuss with you, and a dressing to cover the area for 5 to 7 days.
Contact us
Call the nurse or department looking after you if you’re worried about your port.
IV Therapy/Outpatient Parenteral Antibiotic Therapy (OPAT) Team
- 01296 315485 – Mondays to Sundays, 8.30am to 4.30pm
- 07810 181584 – Bank Holidays, 9am to 4.30pm (on call basis)
Cancer Care and Haematology Unit, Stoke Mandeville Hospital
- 01296 315125 – Mondays to Fridays, 9am to 5pm
Sunrise Cancer Unit, Wycombe Hospital
- 01494 426238 – Mondays to Fridays, 9am to 5pm
Ward 5, Stoke Mandeville Hospital (24 hours)
- 01296 316336
Acute Oncology Team
- 01296 315139 – Mondays to Fridays 8am to 6pm
Stoke Mandeville Hospital A&E
- 01296 315664
