Stroke Unit
Information for patients and carers about the Stroke Unit at Wycombe Hospital.
Calling the Stroke Unit
Where possible please arrange for one person to be the main point of contact. We are unable to provide detailed medical information over the telephone.
- Hyperacute Stroke Unit (Ward 8): 01494 426113
- Acute Stroke Unit (Ward 9): 01494 425080
Visiting times
Visiting times are restricted so that patients have time to participate in rehabilitation and get sufficient rest. Visiting times are posted on the main doors to each ward.
Our location
The Stroke Unit is located on Floor 2 at Wycombe General Hospital, Queen Alexandra Road, High Wycombe, HP11 2TT.
The Unit is located in the Green Zone (Rear Building). The nearest entrance is Main Entrance 1.
A stroke happens when the blood supply to part of the brain is cut off.
It may be caused by:
- Bleeding in or around the brain (haemorrhagic stroke)
- A blockage within a blood vessel (ischaemic stroke)
Affected brain cells cannot get the oxygen they need to survive, resulting in changes to how you move, think, feel, and communicate.
A ‘mini stroke’, known as a transient ischaemic attack (TIA) is when there is a temporary blockage to a blood vessel in the brain. This also needs investigating because it may indicate an increased risk of future stroke.
The signs of stroke
Different parts of the brain control different parts of the body, so symptoms will depend on the brain area affected and how much damage has been done.
The main stroke symptoms can be remembered with the word FAST:
- Face – the face may have dropped on one side, the person may not be able to smile, or their mouth or eye may have drooped.
- Arms – the person may not be able to lift both arms and keep them there because of weakness or numbness in one arm.
- Speech – their speech may be slurred or garbled, or the person may not be able to talk at all despite appearing to be awake; they may also have problems understanding what you’re saying to them.
- Time – it’s time to get medical help immediately if you notice any of these signs or symptoms.
Other symptoms include: paralysis down one side of the body; sudden loss or blurring of vision; being/feeling sick; dizziness; confusion; difficulty understanding language; problems with balance/co-ordination; difficulty swallowing; a sudden and very severe headache; loss of consciousness. However, please be aware that these symptoms can have a range of causes.
You have been admitted to the Stroke Unit because it is suspected that you have had a stroke.
The Stroke Unit is located at Wycombe Hospital and is the NHS’ centre for stroke care within Buckinghamshire. We offer 24/7 care on two adjacent wards:
- the Hyperacute Stroke Unit (HASU; Ward 8)
- the Acute Stroke Unit (ASU; Ward 9)
Treatment for stroke
The sooner you can get help for a stroke, the more likely you are to make a better recovery.
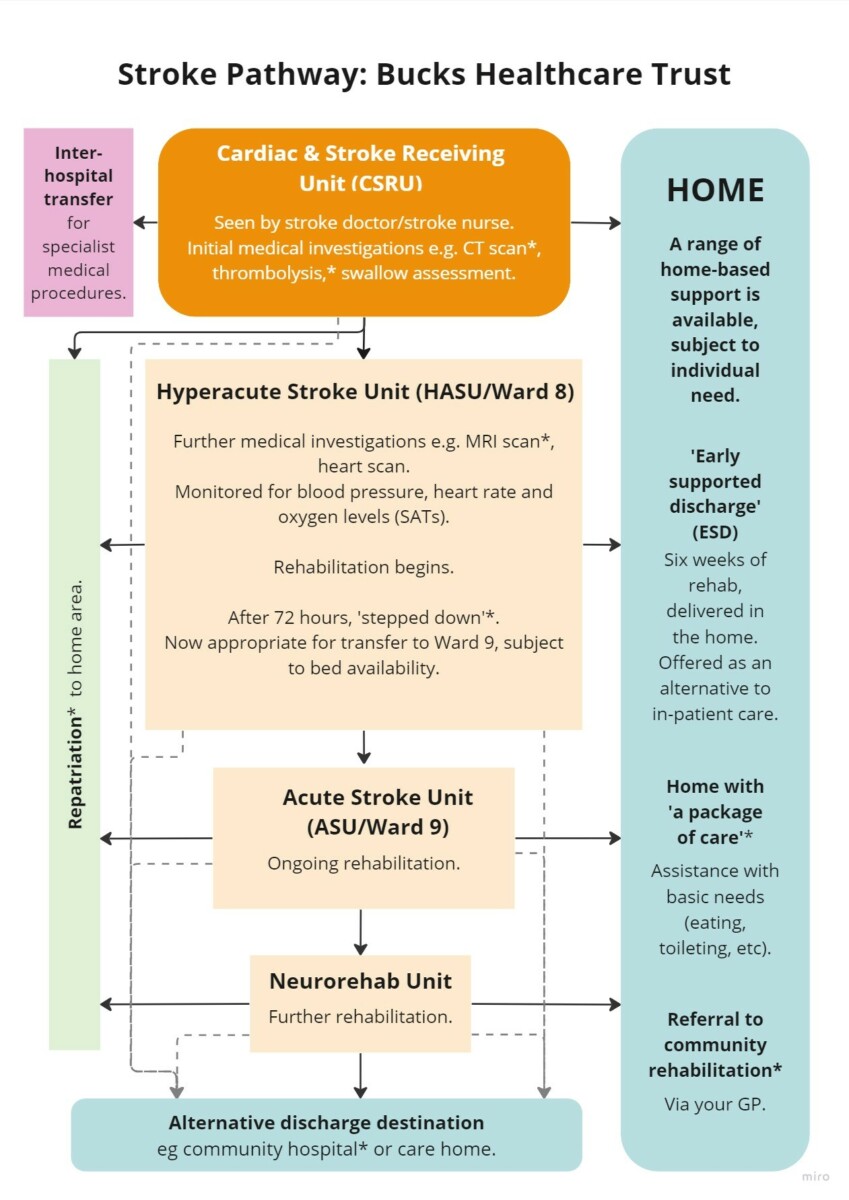
As a new patient, you will first be admitted to the Hyperacute Stroke Unit (HASU). Here, our priority will be to assess your health swiftly so that we can treat your stroke and work to prevent it happening again.
Within 24 hours of your admission, you’ll have a CT scan or an MRI brain scan. This will help us to try to find out:
- The location and amount of damage that may have been made to your brain.
- The cause of the stroke.
Depending on the scan results and the amount of time since the stroke occurred you may be offered:
- Surgery – an operation to remove a blood clot from your brain (thrombectomy), or to reduce pressure in the brain (craniotomy)
- Medicines to dissolve blood clots (thrombolysis), or to reduce blood pressure, etc.
Find out more information about treatments for stroke on the NHS website.
| CT scan | A computerised tomography (CT) scan uses X-rays and a computer to create detailed images of the inside of the body. CT scans are sometimes referred to as CAT scans. They produce detailed images of many structures inside the body, including the internal organs, blood vessels and bones. |
| Community hospital | A small local hospital that provides a range of services, such as diagnostics, treatments, rehabilitation, and end-of-life care, to the local community. |
| Community rehabilitation | Rehabilitation that takes place outside of acute hospital wards. |
| MRI scan | A magnetic resonance imaging (MRI) scan uses strong magnetic fields and radio waves to produce detailed images of the inside of the body. An MRI scanner is a large tube that contains powerful magnets. |
| ‘Package of Care’ (POC) | This consists of carers coming into the home to assist with certain activities as identified by the rehabilitation team. Examples include cleaning, washing, dressing, and feeding. May be funded by social services or privately. |
| Rehabilitation | The restoration, to the maximum degree possible, of an individual’s function and/or role, both mentally and physically, within their family and social networks, and within the workplace where appropriate. |
| Rehabilitation Units | Can be a dedicated ward within a community hospital or a standalone unit. For medically stable patients who may benefit from ongoing inpatient rehabilitation. Referral to such units is decided on a case-by-case basis by the clinical team. |
| Repatriation | Transfer of patient to their local hospital. This is dependent on the address of your GP. |
| ‘Stepped down’ | The patient no longer requires intensive monitoring of health status. |
| Thrombolysis | Use of medicines to dissolve blood clots. |
Your medical care will be overseen by a Consultant leading a team of Doctors and sometimes Physician Associates. They will confirm your diagnosis and discuss treatment options. They will also meet regularly with members of the multidisciplinary team (see the table below) to discuss goals and progress.
| ROLE | UNIFORM |
| Nurses – monitor and manage your health, for example, by measuring your heart rate and giving medicines as prescribed by medical team. | Blue tunic with white piping |
| Specialist stroke nurses – specialist nurses who provide information and support for patients and their families, for example by explaining brain scan results with you. | Dark blue tunic with white piping |
| Healthcare assistants – assist you with daily living activities on the ward, for example, washing, dressing and eating. | Grey |
| Physiotherapists – help you improve your movement and mobility. | White tunic with navy blue piping. |
| Occupational Therapists – help you manage your ability to do everyday tasks. | White tunic with green piping. |
| Speech and Language Therapists – help you with eating/drinking difficulties and/or communication difficulties. | White tunic with purple piping. |
| Dietitians – provide nutrition and dietary advice. | White tunic with royal blue piping. |
| Clinical Psychologist – provides support (to patients and families) and management of difficulties with mood and cognition. | No uniform |
| Clinical support workers – carry out therapy/monitor programmes designed by physiotherapists, occupational therapists, speech & language therapists and dietitians. | White tunic with white piping |
| Housekeeper – provides meals/drinks and snacks. | Pale green tunic top |
Other professionals you may meet in hospital:
- Cardiologists – manage conditions relating to the heart.
- Urologists – manage conditions relating to kidneys and bladder
- Diabetic nurses – help patients manage their blood sugar levels.
- Endocrinologists – manage conditions relating to hormones, hormonal glands, and associated tissues.
- Gastroenterologists – manage conditions related to digestive system and liver.
- Orthoptists – evaluate and treat visual difficulties.
Meet and greet meetings
Within around 10 days of your admission, we aim to invite patients and their carers to a ‘meet and greet’ meeting. This meeting is usually attended by representatives from the medical team and the therapy teams involved in your care.
Family meetings
Subsequent ‘family meetings’ can be arranged at any time. They will be arranged at intervals during your admission, usually via your key contact (see below) and provide an opportunity to gain feedback on progress, ask specific questions or discuss future plans and discharge.
Key contact
We allocate a key contact to all patients on admission to the Stroke Unit. The name or role of your key contact should be in your Stroke Association Patient Pathway booklet or on the board above your bed.
This role is usually carried out by one of the therapy teams working with you, for example a physiotherapist. They will coordinate any questions you might have for the multidisciplinary team. Ask for your key contact on either the HASU or ASU ward.
Specialist Stroke Nurses
We have a dedicated specialist stroke nurse on each ward. They support, inform and advise patients and their carers about your diagnosis, treatment, and prognosis. The specialist nurses can talk through the results of brain scans and discuss the type (haemorrhagic or ischaemic) and location of your stroke.
Please ask for the specialist nurse on either the HASU or ASU ward.
Community Stroke Coordinator
We aim to provide an integrated service, offering a smooth transition from the acute setting in hospital to the community setting. If you have any queries about community services after discharge, please contact the Community Stroke Coordinator on 07917 073614.
Stroke affects everyone differently. Some people may experience only mild effects, while for others the impact may be more severe and long-term.
You’ll be at the centre of your own rehabilitation journey. We ask about what matters most to you, and help you work towards this. We’ll encourage you to do as much as you can for yourself so that your every activity is part of your road to recovery and independence.
The following information describes some of the changes commonly experienced after a stroke. However, this is not a complete list. If you are experiencing other symptoms, please mention this to a member of staff.
How does the brain get better?
The brain gets better after a stroke by reorganising the connections between brain cells.
For example, if you drive from A to B and a road was closed, you’d need to find another route to reach your destination. For this to happen, the body and brain must practise everyday tasks over and over again.
Mobility, sensation and movement
The physical effects of stroke can affect everyday abilities such as balancing, walking, holding things, and continence. Fatigue, pain, and changes to sensation are also frequently reported. To help you manage these difficulties, Physiotherapists will help you move your muscles and safely build your strength.
Eating and drinking
Following a stroke many people experience difficulties with swallowing (dysphagia). If this affects you, Speech and Language Therapists (SLTs) will work with you to introduce food and drink safely. Working alongside Dietitians, SLTs may recommend a modified diet, such as pureed food or thickened fluids. Dietitians will assess, advise and provide ongoing monitoring to ensure you receive adequate nutrition to support your recovery and rehabilitation. If you have longer term swallowing difficulties the dietitians will discuss alternative modes of feeding with you.
Communication
After a stroke, your speech may be slurred (dysarthria), disorganised (apraxia of speech), and/or you may find it difficult to understand language or express yourself (aphasia). If this applies to you, Speech and Language Therapists will work with you to improve your speech and language abilities. They may also help you learn other ways to communicate and support families to make conversations with loved ones easier.
Thoughts, feelings and behaviour
‘Cognitive’ (thinking) difficulties experienced after stroke can affect memory, thinking speed, concentration, or visuospatial skills (understanding visual information). Emotional and behavioural changes can also occur, with some people displaying strong mood swings (lability), anger, impulsivity, and depression. If you’re experiencing any of these changes, please mention this to a member of staff. The team may refer you to the Clinical Psychologist for support with these issues.
Managing everyday activities
Occupational Therapists will work with you to maximise your independence. They will encourage you to have a go at everyday things, such as washing, dressing, making your own drinks, going to the toilet, brushing your teeth and hair, and eating and drinking. They may also suggest environmental changes to improve accessibility, or provide equipment, such as wheelchairs.
Once you are medically stable, the clinical team will talk with you about the arrangements for any ongoing healthcare you may need.
Decisions regarding your transfer from the Hyperacute Stroke Unit to the Acute Stroke Unit, your home, or another location, will be decided based on a range of factors. These include:
- The stability of your medical health
- The effects of your stroke
- The support and facilities available to you at home
Discharge from hospital
The multi-disciplinary team will work closely with you and your family, where appropriate, to ensure that everything is in place for your discharge. Wherever possible it is our goal to discharge you to your own home. The team may carry out an access visit and other assessments to look at your home and establish what adaptations/equipment/package of care you may need.
The team may start talking about discharge planning early on in your admission – this is to ensure a smooth transition and to have everything in place when you require it. Further assessments, such as seating and social work may be carried out at home after discharge.
Support in the community
Some people may remain in hospital for a number of weeks while they have rehabilitation. However, care and rehabilitation is also available in the community for those who need it. This can include:
- Early Supported Discharge (ESD). This service is available for up to 6 weeks and is an alternative to ongoing inpatient rehabilitation. Where patients meet the criteria they are able to continue their rehabilitation journey at home with therapy input.
- Community Services. At any time after leaving hospital, you can ask your GP for a referral to rehabilitation services (for example: Physiotherapy, Occupational Therapy or Speech and Language Therapy)
Please also consider contacting any of the many community groups who offer information and advice about stroke. Two national organisations are:
- The Stroke Association (www.stroke.org.uk), Tel: 0303 3033 100
- Different Strokes (www.differentstrokes.co.uk), Tel: 0345 130 7172
- Headway (www.headway.org.uk), Tel: 0808 800 2244.
A list of local stroke support groups is also available from the rehabilitation team.
Meal times
Breakfast: 07.30; Lunch: 12.00-13.00; Dinner 17.30.
If you would like a relative or friend to assist you during mealtimes, please discuss this with a member of staff.
We request that visitors do not bring in food for relatives or other patients unless this has been specifically agreed with the ward. A number of people will be on specially modified diets and providing food outside these diets may cause risk to patients with swallowing difficulties.
Personal possessions
Please make sure you have any glasses, dentures or hearing aids with you. You are encouraged to bring in loose-fitting night and day clothes, as well as your own toiletries. Personal laundry will need to be collected and washed by your visitors. We advise that valuables are kept at home.
Mobile phones and other electronic devices
When using your mobile phone or other electronic device on the ward, please be mindful of fellow patients, and use headphones or turn down the sound where possible. Public WiFi is available – select ‘BHT_Public’.
Single-sex accommodation
We try to maintain single-sex accommodation wherever possible. However, due to the need to ensure urgent provision of care for all, on HASU this is not guaranteed.
Consent
Please know that the decision to participate in treatment or therapy remains yours. You have a choice. If a member of staff asks you to agree to something, it is within your rights to say no, or to ask for more information.
Translation and signing services
A translation service is available for patients who do not speak fluent English. Specialist services are also available to support patients with hearing impairment.
Pastoral, spiritual and religious needs
These are met by hospital chaplains who make regular visits to both wards.
Wellbeing services
- The stroke garden is well used during the warmer months, especially for rehab sessions and to meet with family/friends.
- Day rooms with a television, books and board games are available on HASU and ASU.
- The Stroke Units receives a weekly visit from a Music Therapist and a ‘Pets As Therapy’ (PAT) dog.
To help us improve the care we provide to patients, please consider joining the stroke forum. Open to former patients and their family members, the forum meets at Wycombe Hospital four times each year to discuss a range of topics and plan service development projects. In fact, this very booklet came about as a direct result of feedback provided at the forum!
To find out more, please ask your key contact for more information.