Looking after your peripherally inserted central catheter (PICC)
Read our guide below about looking after your peripherally inserted central catheter (PICC)
You can also download a PDF version of this patient information by following the link on the right.
The most effective way for you to receive your treatment is through a peripherally inserted central catheter. It’s often called a PICC line.
What is a PICC?
It’s a long, flexible tube, often called a line, which is inserted into a large vein in your upper arm. It’s threaded up your arm until the tip sits in a large vein just above your heart.
The PICC is made of a thin, soft, non-irritant material so it can be left in place for weeks or months depending on how long you need it. This means you can have your treatment without needing more needles inserting into your veins.
A PICC can help give treatments such as intravenous feeding (Total Parenteral Nutrition (TPN)), chemotherapy and antibiotics. It can also be used to take blood samples or give blood transfusions.
How is the PICC inserted?
A specially trained nurse or health professional will put the PICC in place, either in hospital or as an outpatient. They’ll use local anaesthetic to stop any discomfort during the procedure. Once in place, they’ll use a securement device (Securacath – orange clip) and a clear dressing to keep it in place.
It will be confirmed that your line is in the correct position on insertion or you may need a chest x-ray.
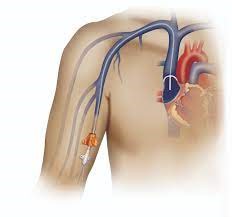
PICC line threaded through the vein

End of the PICC line secured with a dressing
Possible risks and complications
Every procedure has potential risks and complications. Before we insert the PICC we’ll fully explain these risks to you.
We’ll ask you for your consent before going ahead.
Tell your nurse or doctor after you have the PICC inserted if you have:
- ongoing bleeding or discharge at the PICC entry point
- swelling, redness or pain anywhere in your arm, chest or neck
- a temperature or feel feverish
- increased redness around the entry point (see the visual infusion phlebitis (VIP) table below)
Visual infusion phlebitis (VIP)
Use the table below to monitor any increased redness around the PICC entry point.
| VIP score | Description | Example | Action |
| 0 | Healthy site, no signs of phlebitis |  |
Continue routine monitoring |
| 1 | Pain or redness at site |  |
Tell the OPAT/IV team/unit and monitor the site |
| 2 + | Pain and redness, swelling or any pus |  |
Tell OPAT/IV team /unit and get a medical review |
Looking after your PICC
Once in place, you must take care of your PICC to stop it from coming out or getting infected.
Wash your hands
If you ever need to handle your PICC, always wash your hands with soap and water and dry your hands thoroughly first.
Keep the dressing clean and dry
Once a week, a health professional will clean the area where the line goes into your skin and change your dressing and bung at the end of the line
If at any time your dressing becomes loose or detached from your skin, try to secure the line with tape or a bandage. Contact your unit/nurse to arrange for a new dressing as soon as possible.
Check your line daily
To help monitor the site where we insert your line, your nurse may give you a VIP chart, or see the chart above, to check the site daily.
If you can see more than one line coming out of the insertion site, the PICC may have moved.
Tell your nurse. You may need to have another chest x-ray to re-check the position.
Baths and showers
You can do both. Do not soak your arm underwater. Always dab the dressing dry if it gets wet.
You can wrap clingfilm around the waterproof dressing for extra protection or buy a specialist arm protector. Talk to the unit or team for more information
Swimming
You should never swim or use hydroptherapy with a PICC in place.
Exercise
Don’t play sport like golf or do upper body weight lifting as the PICC may move. You can do normal daily activities as usual.
How is the PICC removed?
A nurse will do this either at your home or in the outpatient department in hospital.
They’ll gently ease out the PICC and remove the securacath. You may feel a bit of discomfort for a few minutes. You’ll have a dressing applied to the break in your skin, which you need to leave on for 24 to 48 hours before removing it.
If you have any questions
Contact the nurse or department where you’re getting your treatment. They’ll talk to you about your concerns and if necessary, check your line.
How can I help reduce healthcare associated infections?
Infection prevention and control is important to the wellbeing of our patients so we have procedures in place. Keeping your hands clean is an effective way of preventing the spread of infections.
You, and anyone visiting you, must use the hand sanitiser available at the entrance to every ward before coming in and after you leave. You may need to wash your hands at the sink using soap and water. Hand sanitisers are not suitable for dealing with patients who have symptoms of diarrhoea.
More help or advice
Contact our patient advice and liaison service (PALS) on 01296 316042 or bht.pals@nhs.net
About our patient information
We aim to make the information as up to date and accurate as possible, but please note that it’s subject to change. You must always check specific advice on any concerns you may have with your doctor.
Contact us
IV Therapy Nurse/OPAT
Cancer Care and Haematology Unit, Stoke Mandeville Hospital
Ward 5, Stoke Mandeville Hospital
Acute Oncology Team, Stoke Mandeville Hospital
Sunrise Cancer Unit, Wycombe Hospital
Stoke Mandeville Hospital Accident and Emergency
8.30am to 4.30pm, 7 days a week. Bank Holidays, 9am to 4.30pm
9am to 5pm, Mondays to Fridays
24 hours a day
8am to 6pm, Mondays to Fridays
9am to 5pm, Mondays to Fridays
24 hours a day
01296 315485 / 07810 181584 (Bank Holidays, on-call basis)
01296 315125
01296 316336
01296 315139
01494 426238
01296 315664
