Laparoscopic hysterectomy and assisted vaginal hysterectomy
This leaflet is for women who have been advised to have a laparoscopic (keyhole) hysterectomy. It outlines the common reasons that doctors advise for this operation, potential benefits, as well as risks, recovery from the operation and what to expect when you go home.
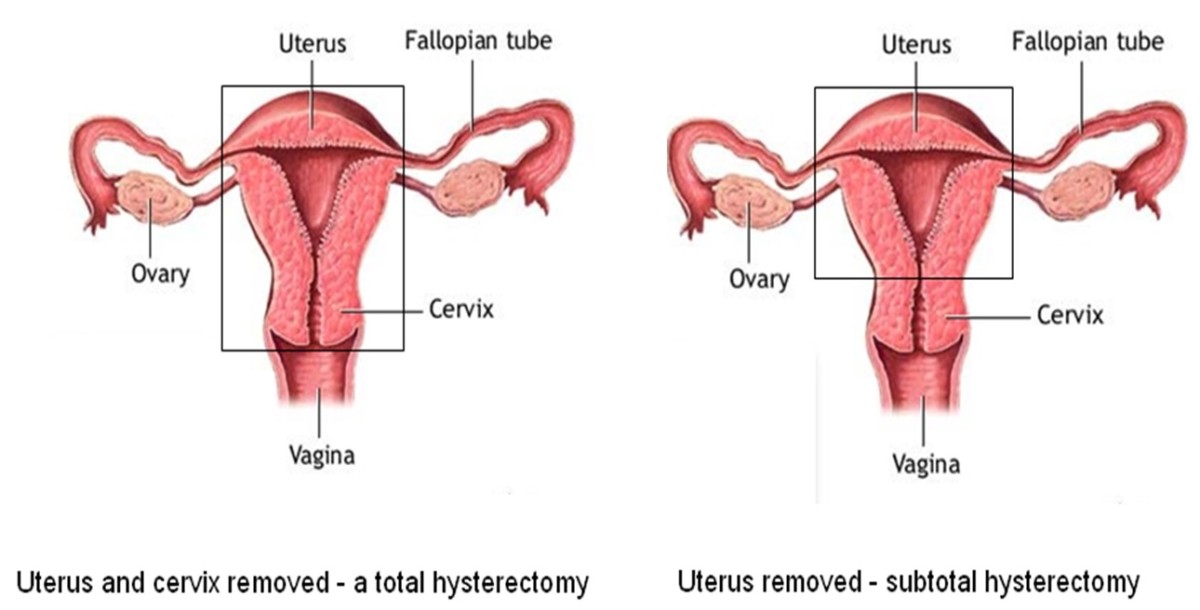
A total laparoscopic hysterectomy (TLH) is the removal of the womb including the neck of the womb by keyhole surgery. A laparoscopic subtotal or supracervical hysterectomy (LSH/LASH) is keyhole surgery to remove the uterus (womb), however, the neck of the womb or cervix is left intact. With this latter type of procedure, you will still need to have routine cervical smear tests.
A laparoscopic-assisted vaginal hysterectomy (LAVH) is a hysterectomy in which some aspects of the hysterectomy are performed by laparoscopic surgery and the operation is completed by vaginal surgery (as for a vaginal hysterectomy).
These operations may be performed with the removal of the fallopian tubes and /or ovaries or leaving them intact.
Why is a hysterectomy necessary?
Women undergo hysterectomies to treat a range of conditions including heavy menstrual bleeding, uterine fibroids, endometriosis, prolapse and cancer.
Hysterectomy is usually a planned procedure that is considered for conditions other than cancer, when other medical or less invasive surgical treatments have failed.
What are the benefits of a keyhole operation?
There are several advantages to having a hysterectomy by the laparoscopic or keyhole approach. These include less scarring, less pain after the operation, a shorter stay in hospital and a quicker return to normal life.
What is the difference between a laparoscopic subtotal and a total hysterectomy?
A subtotal hysterectomy involves removing the body of the womb without the cervix. As a result, the operation is quicker and generally easier and there is a reduced risk of complications including damage to the bladder and the ureters (the tubes draining the kidneys to the bladder). You will also have a smaller risk of developing a vaginal prolapse in the future.
However, after a subtotal hysterectomy, you will still need to have routine cervical smear tests and you will have a small chance of spotting (about 1 in 6) at the time you would have had your periods. The risk of needing further surgery to remove the neck of the womb later is small, about 3-8 in 100 cases.
A laparoscopic total hysterectomy is like a subtotal hysterectomy except that the neck of the womb (cervix) is also removed during the operation. If the hysterectomy is being performed due to a diagnosis of cancer a total hysterectomy will be recommended. It may be an advantage to perform this type of operation when pain is the main reason for the hysterectomy e.g. in cases of endometriosis, or if you no longer wish to have further cervical smears.
Your Doctor will discuss the options with you and help you reach a decision on the appropriate procedure for you.
A visual guide to the female reproductive system
Laparoscopic Total/Subtotal Hysterectomy – How is it done?
Subtotal Hysterectomy
If a subtotal hysterectomy is performed, after freeing the uterus, the body of the uterus is detached from the cervix (the neck of the uterus).
The detached uterus is then usually removed through a small cut in the upper vagina which is closed with dissolvable stitches, or through a small cut in the tummy (usually at the bikini line) which is closed with stitches at the end of the operation. On occasions a thin instrument called a morcellator may be introduced into the abdomen through one of the incision sites.
Morcellation means the gentle cutting up of tissue into small pieces that can then be easily removed from the body after keyhole surgery. To contain the spread of pieces of the (morcellated) uterus, the process of morcellation may be performed within a small bag in the abdomen, which is removed at the end of the operation.
As part of either procedure a thin tube (catheter) is introduced to drain and rest the bladder and will usually be removed the morning after your operation.
You may also have a vaginal pack (a swab) in the vagina to soak up any light vaginal bleeding from the operation. This will be removed the morning after your surgery.
Laparoscopic Assisted Vaginal Hysterectomy (LAVH)
An LAVH procedure involves both laparoscopic and vaginal surgery. Laparoscopy is utilised to perform division of the upper uterine ligaments and occasionally the uterine arteries. The completion of the hysterectomy is performed by vaginal surgery – for further details please refer to information provided by the Royal College of Obstetricians and Gynaecologists: Laparoscopy – recovering well patient information leaflet | RCOG.
What happens if my ovaries are removed before menopause?
If your ovaries are removed at the time of hysterectomy, you may experience symptoms associated with menopause. These include hot flushes, night sweats, difficulty sleeping, vaginal dryness, irritability and/or depression. You may wish to consider hormone replacement therapy (HRT) or other tablets to suppress these symptoms after your surgery. Your doctor will discuss these types of treatment with you during counselling before your surgery.
If your ovaries are not removed, you will continue to have monthly menstrual cycle-related hormone changes and with a subtotal hysterectomy, you may possibly have minor spotting. After a total hysterectomy or LAVH, you should not have any monthly bleeding.
What are some of the general risks associated with a hysterectomy?
Other than anaesthetic risks which are associated with all operations, laparoscopic hysterectomies have a risk of heavy bleeding during the operation and this occurs in about 1% of patients. Infection can occur in up to 1 in 10 patients after a hysterectomy. There is also a small risk of damage to other organs such as the bowel, bladder, and ureters (the tubes draining the kidneys to the bladder). With any surgery there is an increased risk of developing blood clots in the legs and lungs, you will therefore undergo a risk assessment and may be offered blood thinning injections to reduce your risk.
Occasionally it may be necessary to treat complications or to complete the operation via open surgery (laparotomy).
When do I come in and how long would I expect to stay?
All patients will be reviewed by the Pre-Assessment team before the operation takes place. This is an outpatient appointment and is an opportunity for us to ensure you are fit and fully informed prior to the planned operation, for you to ask questions about your procedure and to discuss your aftercare/discharge with the nursing staff. We will carry out routine blood tests and sometimes other investigations, as necessary, before your surgery, for instance, ECG (electrocardiogram) or chest X-ray. The visit usually takes about an hour.
You will normally be admitted on the day of your surgery. Your length of stay depends on a number of factors, but most women can go home 24-48 hours after their surgery if they feel well enough.
What might I expect after surgery?
You may experience some shoulder tip discomfort, which is due to trapped gas from the operation. This will settle quickly, but pain relief medication and peppermint water/tea, along with gentle movements, will help. You may have some initial abdominal discomfort requiring pain relief. If you have a problem with constipation following your operation, please ask for bowel medication to be prescribed along with your pain relief tablets.
Some women might experience some vaginal bleeding and discharge, though usually this is very minimal after a laparoscopic subtotal hysterectomy. However, if your vaginal loss is persistent (longer than 2-3 weeks), becomes heavy with blood clots, or you notice an offensive smell, please contact your GP.
We usually recommend you take things gently for the first week after your operation with no strenuous lifting e.g. nothing heavier than a kettle. However, you should begin walking, if possible, as soon as you get home, gradually increasing to 30-60 minutes a day after 2 or 3 weeks.
Overall you should be able to carry out light activities during the second week and you should be resuming normal activity during the third week.
For more detailed information on recovery after a laparoscopic hysterectomy please refer to the Royal College of Obstetricians and Gynaecologists leaflet: Laparoscopy – recovering well patient information leaflet | RCOG
General Advice
Urine
If passing urine becomes painful or you experience any problems, contact your GP.
Hygiene
You may shower or have a bath the day after your operation. Do not worry about your scars getting wet, pat them dry with a clean tissue or let them air dry.
Driving
You should not drive for 48 hours at least after your anaesthetic. Please seek advice from your insurance company or refer to your insurance documentation before driving.
Sexual Activity
Refrain from penetrative sexual activity for at least 6 weeks to allow for internal wounds to heal.
Lifting and Exercise
Avoid heavy lifting and strenuous aerobic exercise for 2-4 weeks.
Follow Up
There is no routine follow up, however, if you have any problems, please contact the Surgical Floor on 01296 418110 or arrange to see your GP.
Useful Contact Numbers
Wycombe Hospital Ward 12A 01494 426401
Stoke Mandeville Hospital 01296 315000
Ask for Gynaecology Secretaries
Surgical Floor 01296 418110
Wycombe Hospital 01494 526161
Ask for Gynaecology Secretaries
