Hysteroscopy in an outpatient clinic
A hysteroscopy is where a small, fibre optic ‘telescope’ and camera is used to look at the lining and shape of your uterus (womb).
You can have it done in the outpatient department. Or, if you choose to have a general anaesthetic, it will be done in the operating theatre (you will still be able to go home the same day). Please let your doctor know if you would prefer a general anaesthetic.
Deciding whether to have a hysteroscopy
A hysteroscopy can help to find the cause of problems relating to:
- Abnormal bleeding from your uterus
- Heavy or irregular bleeding between periods (inter-menstrual bleeding)
- Irregular bleeding whilst on Hormone Replacement Therapy (HRT)
- Irregular bleeding on Tamoxifen
- Bleeding after sexual intercourse (post-coital bleeding)
- Bleeding after menopause (post-menopausal bleeding)
- Assessing the anatomy of the uterine cavity
- Persistent vaginal discharge
- Fertility issues
Where found, some problems can be dealt with during the hysteroscopy, such as:
- Fibroids (non-cancerous growths of the muscle of the uterus)
- Polyps (non-cancerous soft tissue of the lining of the uterine cavity)
- Thickening of the lining of the womb (the endometrium)
- Removal of displaced intrauterine contraceptive devices (coils)
- Removal of scar tissue/adhesions in the uterine cavity
What are the risks associated with hysteroscopy?
Outpatient hysteroscopy is a very common and safe procedure. However, as with any surgical procedure there is a small element of risk.
Your doctor or specialist nurse will explain the risks to you before you give your consent for the procedure. Please ask questions if you are uncertain.
Risks or complications from this procedure are rare but the following can sometimes occur:
- Pain – the amount of discomfort experienced varies. You may feel a little discomfort (like period pain) as the telescope goes through the opening of the cervix. This is why we advise taking pain relief at home before your appointment. If you are unable to tolerate the pain, just say so and the procedure can be stopped.
- Feeling faint or sick – this feeling may continue after the procedure, and you may need to rest for the remainder of the day.
- Bleeding – this is usually light and only rarely heavy.
- Infection
- Uterine perforation (damage to the wall of the uterus). The risk of perforation is rare and this risk is lower (less than 1 in 1000 cases) during outpatient hysteroscopy compared with hysteroscopy under general anaesthetic.
- Damage to your cervix – this risk is rare
- Difficulty seeing the cavity of the womb
- Failure to complete procedure – this is usually due to the development of pain or problems getting into uterine cavity.
As the procedure involves inserting surgical instruments into the uterus, this can very occasionally result in injury. It is rare to have excessive bleeding, perforation (puncture) of the uterus or an infection. About two out of every 1,000 patients have complications and these are dealt with appropriately. If you have any concerns about the procedure, please ask.
About the procedure
Before your hysteroscopy the clinician performing the procedure will discuss what will happen so you can provide your consent. By giving your consent you agree to have the treatment and confirm that you understand what is involved.
We will give you a gown to wear during the procedure and ask you to undress from the waist down. There will be two or three healthcare professionals in the room and one of them will support you throughout the procedure, helping to make you feel as comfortable as possible. You will be awake all the time. Please don’t hesitate to tell the doctor or specialist nurse if you feel discomfort or pain and wish to stop the procedure.
You will be positioned on the gynaecology couch and made to feel comfortable. We will do our best to maintain your dignity. You will be asked to rest your legs on two foot supports on either side of the couch.
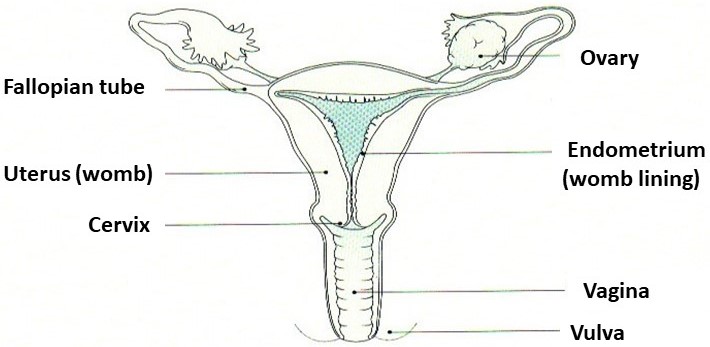
An antiseptic solution is used to clean the surface of the vulva (outside of the vagina). We aim to use a ‘no touch technique’ (vaginoscopy) which does not require use of a speculum (a medical instrument routinely used during smear tests) to enter the cervix (neck of the womb) – this is to minimise discomfort. Sterile fluid will be inserted to help us get a clearer picture. You will feel wet as the fluid trickles out of the vagina.
However, sometimes a speculum examination will be necessary. If you find speculum examination painful, please let us know.
We then insert a telescope to see pictures of the inside of your uterus on our screen – you can watch the screen if you wish to. Some sterile fluid is inserted to help us get a clearer picture. The actual procedure will only take a short time.
A small number of women may need some local anaesthetic to relax the neck of their womb.
We may then remove a tiny sample of your womb lining. This tissue is called a biopsy and will be examined in the laboratory. If we find any small polyps, they can also be removed during the procedure and sent away for assessment.
Before your hysteroscopy
Pregnancy
Make sure you don’t become pregnant before a hysteroscopy. You can do this by ensuring you use barrier contraception (condoms or a diaphragm) from the first day of your last period before the hysteroscopy, right up until the day of the appointment itself.
On the day of the procedure, we may ask your permission to do a pregnancy test. You may need to give a urine sample for this.
Your procedure will be postponed if there is any possibility that you might be pregnant.
Your period
If you are menstruating or are due to be menstruating at the time of your hysteroscopy don’t worry. Unless you have particular objections, it is usually still possible to proceed.
Eating, drinking and medicines
- You can eat and drink as normal and take your usual medicines.
- If you are taking warfarin tablets, please have an INR blood test within a week of the procedure date – as the level needs to be less than 3 – if not your hysteroscopy may be cancelled. If you are taking one of the Direct Oral Anticoagulant Drugs (Apixaban, Dabigatran, Edoxaban, Rivaroxaban) your doctor will advise you.
- We recommend you take mild pain relief at least 1 hour before your appointment either:
- 1000mg (2 x 500mg tablets) Paracetamol or
- 400mg (2 x 200mg tablets or 1 x 400mg tablet) Ibuprofen.
This will help to prevent/reduce period type discomfort during and immediately after the procedure.
What you should bring with you:
- a sanitary towel
- something to read while you wait for the procedure
- a CD of your choice if you feel this will help you to relax
You can also have a friend or relative with you.
When you arrive
Please go to Outpatients and book in at reception. Ask for the Hysteroscopy Clinic. You will be asked to wait until you are called into the clinic by the nurse.
Your visit to the hysteroscopy clinic should take no longer than two hours (usually less than one hour).
Following the procedure
Results:
- You will usually be told the findings before you leave.
- If a biopsy has been taken or other tissue (for example, a polyp) is removed, these results take longer as they are sent to a laboratory for analysis. We will write to you with the results within approximately one month.
Bleeding:
- It is common to experience abdominal cramps, a bit like period pain. You may also have bleeding following the procedure. This occasionally can be heavy. The blood loss usually settles within 24-48 hours, but you may need sanitary protection for up to a week. We advise you to use sanitary towels/pads. Please do not use tampons. If you find that the bleeding continues to be heavy or you experience acute pain, please contact your GP.
- Where any additional treatment has been carried out, then the bleeding and/or discharge may be a little heavier and last longer.
- It may be useful to have a small supply of pain relief. We recommend you have a relative or friend drive you home after your appointment.
Sexual intercourse: can be resumed once the bleeding and/or discharge has stopped.
Are there any alternatives to outpatient hysteroscopy?
There are two other options:
- You may choose to have the hysteroscopy under general anaesthetic. This will be done in an operating theatre, usually as a day case procedure.
- You can have an ultrasound scan to look at your womb. This does not provide as much detailed information as the hysteroscopy and you may already have had an ultrasound before being referred for a hysteroscopy.
Contact the hysteroscopy team
Please call the hysteroscopy office on 01296 316239
The office is open from 9:30am – 1:30pm Monday, Wednesday, Thursday and Friday. It is closed on Tuesdays.
- Call the team for any queries about your appointment or procedure.
- Or if you need an independent interpreter, please call the team before your appointment. Please note: The use of family or friends as interpreters is not recommended by the Trust. Interpretation services have been shown to improve patient satisfaction.
Other useful numbers and websites:
- Patient Advice and Liaison Service (PALs): 01296 831120
- NHS 111 offers medical help and advice from fully trained advisers supported by experienced nurses and paramedics. Available over the phone 24 hours a day.
- NHS website provides online information and guidance on all aspects of health and healthcare, to help you make choices about your health. nhs.uk
- rcog.org.uk/en/patients/patient-leaflets/outpatient-hysteroscopy/