How to take Plenvu bowel preparation before a colonoscopy
Read our guide below which explains how to take Plenvu bowel preparation before a colonoscopy
What is Plenvu?®
It’s a polyethylene glycol (PEG) laxative designed to cleanse your bowel before your planned colonoscopy. It causes you to have diarrhoea, or frequent bowel movements. You’ll start passing brown liquid and this will gradually change into a clear/yellowish liquid.
A clean bowel will allow a clear view of the inner lining which is important for accurate diagnosis and treatment.
Please ensure you follow the instructions carefully. We may need to cancel the colonoscopy and repeat it at another time if the bowel isn’t clean enough.
Do not take this medication if you don’t think you’re fit enough to go backwards and forwards to the toilet. Contact the doctor or team who referred you for this test for further advice.
What should I do before taking Plenvu®?
Follow a low fibre diet for 3 days before taking Plenvu®. See our low fibre diet leaflet for details of the type of diet you need to follow.
How do I take Plenvu®?
Plenvu® is a two-dose preparation.
Dose 1 is a single mango-flavoured sachet.
Dose 2 is two sachets (A and B) fruit punch flavoured.
Take all sachets with the right amount of water according to the timing.
Oral medication should NOT be taken within one hour of taking Plenvu® as it may not be absorbed properly – please see the table below:
| MEDICINE | INSTRUCTION | ADDITIONAL DETAILS |
| Iron Tablets | Stop 7 days prior to taking Plenvu® | |
Anticoagulants and anti-platelets (blood thinning medication) including:
|
Tell the booking team who makes your appointment. They can arrange a pre-assessment consultation and advise you how to prepare for your test. | Call 01296 831210 |
| Insulin controlled diabetes patients |
Please see supplementary information sheet and contact your Diabetes Specialist Nurse/ or GP Practice Nurse for further advice if required. | Glucose energy drinks and glucose tablets if sucked can be taken for hypoglycaemia.
You will need to manage a reduction in your normal insulin dose during bowel preparation and until after your procedure |
| Oral anti-diabetes tablets | Please see supplementary information sheet and contact your Practice Nurse at your GP surgery for further advice if required. | Absorption of tablets may be affected by the Plenvu®. |
| Diet controlled diabetes patients | No action required | |
| All diabetic patients must talk to the booking coordinator to arrange an appropriate appointment time.
01296 831210 |
||
| Anti-epileptics, oral contraceptives, antibiotic and oral anti-diabetic medication | Bowel cleansing may interfere with normal absorption of these drugs. | Contact the Medicines Resource Centre for further advice. |
| Anti-diarrhoeal tablets | Stop 3 days prior to taking Plenvu® | |
When should I NOT take Plenvu®?
Do not take Plenvu® if your condition has significantly changed since you were referred for this treatment, or if you’ve developed any of the symptoms listed below.
Contact the Endoscopy unit where you’re booked to have your procedure for further advice.
Do not take Plenvu® if you have:
- a possibility that you’re pregnant
- heart failure
- had a heart attack within the last 6 weeks
- kidney failure
- difficulty in swallowing
- severe breathing problems
- a stomach or bowel blockage
- had recent bowel surgery (within the last 6 weeks)
- active diverticulitis (this means that you will have pain and a doctor may have given you antibiotics).
How to make up Plenvu®
Plenvu® may be easier to take if:
- You drink through a straw.
- It has been refrigerated after it has been made up
- It is sipped slowly rather than drinking it quickly
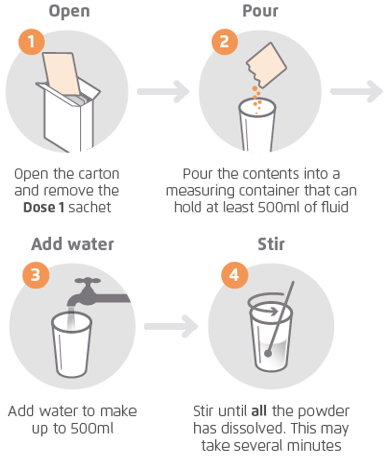
Making up Plenvu® dose 1
You should make up Plenvu® Dose 1 when you need it, based on your dosing schedule (see below).
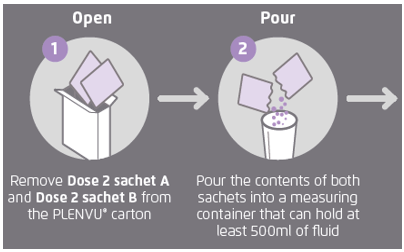
Making up Plenvu® dose 2
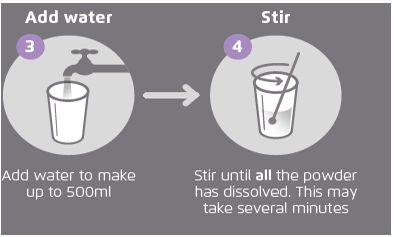
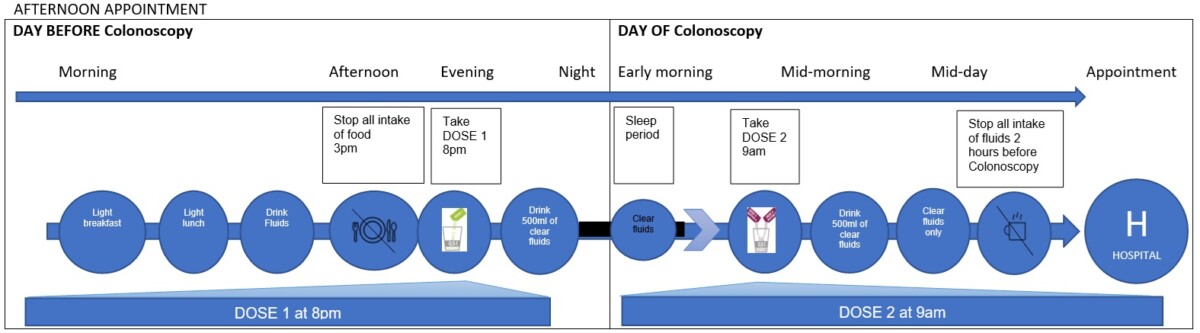
How to take Plenvu® – timings
The timing of your Plenvu® doses depends on whether you are having a morning (before 12.00 noon), afternoon (after 1pm) appointment. Please follow the relevant row on the timeline below depending upon your appointment time. Stop eating by the time shown on the timeline.
Clear fluids may be taken until 2 hours before the procedure.
Suggested fluids include water, cordial, squash (not blackcurrant) or herbal tea of your choice – these need to be taken after each sachet of Plenvu®.
Morning appointment
Care after taking Plenvu®
- Use a barrier cream to prevent a ‘sore bottom’, e.g. petroleum jelly
- Make sure you allow enough time to travel to the hospital for your colonoscopy
- Consider using wet wipes after each bowel movement. Wet wipes that have been refrigerated are particularly soothing.
You can also download a PDF version of this patient information by following the DOWNLOAD link on this page.