Hospital at Home programme: Monitoring respiratory patients at home
Bucks Integrated Respiratory Service (BIRS)
Hospital@Home programme: Monitoring Respiratory Patients at home
Watch a short video about this service:
This patient advice guide is for patients who have one of the following conditions and for whom it has been decided to continue their care through the Hospital@Home programme:-
- Coronavirus (Covid-19) or another viral or bacterial chest infection.
- Respiratory condition such as COPD, Asthma or Interstitial lung disease.
- Oxygen weaning – an admission to hospital that requires short term use of oxygen therapy on discharge in your home to assist with your recovery.
You will be monitored through the Hospital@Home programme for approximately two weeks.
You will have been supplied with the equipment to take home with you. This will be on a short term loan for the duration of the home monitoring.
We will ask you to check your blood pressure, temperature, pulse and oxygen levels then submit your readings using Doc@Home (a digital platform).
There are also a set of questions to answer which relate to your respiratory condition.
We will need to monitor your symptoms until they improve and the BIRS team will advise you when you are ready to be discharged from the Hospital@Home programme.
A BIRS team member will explain how to use the equipment and the digital platform.
Please note: The equipment is cleaned between use by each patient by NHS staff according to the manufacturer’s instructions.
How to submit your readings
The BIRS Hospital@Home programme uses Doc@Home, (a digital platform), to collect vital sign readings for patients. When you first join the programme we will ask you how you would like to share your readings with the monitoring team.
Readings will be given to the team in one of four ways:
- Web Based Submission – You can sign-up on a web-based version of Doc@Home.
- Smartphone App – You can download the Doc@Home App onto your smartphone or tablet.
- Text Message – Oxygen Weaning patients only
You will receive a text message once a day to your mobile from Doc@Home requesting your readings. When you receive each text, you will be asked to submit your readings by return text in a specified format. - Call from the team – If the above options are too difficult for you the team will speak to you about an alternative solution that works for both you and the BIRS team.
How to check your Blood Pressure
Preparing to take your readings
30 minutes before taking your blood pressure you should avoid the following:
- Alcohol
- Smoking
- Caffeine
- Hot baths or showers
- Large meals
- Exercise
- Restrictive clothing
Taking your blood pressure reading
- Sit upright in a chair with your back against the back of the chair. Place your feet flat on the floor.
- Rest your arm on a table and make sure your arm is relaxed.
- Apply the cuff to the upper part of your Left or Right arm.
- Make sure the air tube is on the inside of your arm and wrap the cuff securely so it cannot slip around.
- The tube side of the cuff should be 1-2 cm above the inside elbow.

- It is important that not to clench your fist when you are taking your blood pressure.
- When you check your blood pressure, do not talk, just relax.
- To start the machine press the blue start button.
- You will feel the cuff inflate quite rapidly. It may temporarily be a bit tender or uncomfortable as the cuff inflates, but this will only be for a short period of time, and the cuff will deflate automatically. If it is too tender/uncomfortable you can press the ‘Stop’ button and the cuff will instantly deflate. Wait a few minutes and retry the measurement.
- Make a note of the results on the screen so you can submit them by your chosen method on Doc@home.
- A few minutes after you have taken your blood pressure, it is sometimes a good idea to check it again, to ensure the readings are similar and accurate.
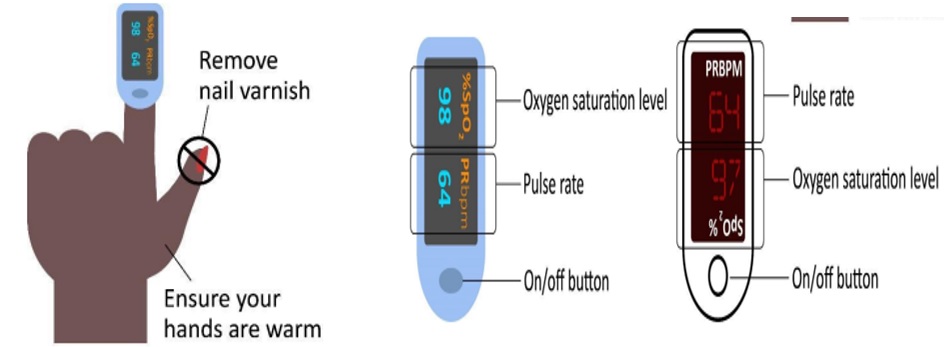
How to check your oxygen saturations and pulse using a pulse oximeter
- Remove any nail varnish or false nail before attaching the probe.
- Clip the oximeter onto your finger.
- Wash your hands before and after use.
- Make sure your fingers are warm.
- After 5-10 seconds, the probe will give you two different numbers – an oxygen saturation level (abbreviated to SpO2) and a pulse rate (abbreviated to PR or BPM)
- We need both readings.
- When the numbers on the pulse oximeter have stopped write the numbers down so you can submit them by your chosen method on Doc@home.
How to check your temperature using the digital thermometer
IMPORTANT: Please do not clean the thermometer.
The thermometer must never come into contact with any fluids.
The thermometer you have been loaned will come supplied with a few disposable probe covers, which minimize the risk of bacterial and contaminant transfer. As only you will be using the machine you do not need to throw away the probe cover each time you use it, but it does need to be put on and taken off each time you take your temperature, otherwise the machine will not work.

- Push the head of the device into a probe cover until it clicks into place. Do not touch the probe cover.
- Once in place, press the larger button.
- Insert the probe into the ear canal – do not push it in too deeply.
- The device will beep when the reading is ready.
- Remove the device from the ear canal and read the temperature display immediately. Make a note of the reading.
- You should normally wait at least 2 minutes before repeating the reading if using the same ear.
- Remove the probe cover by pressing the eject button and keep for use next time.
- If the cover is visibly dirty or damaged then throw it away and use a new one next time.
- Replace the thermometer back into its base unit. It will turn off automatically when it is in the base.
If you would like more information, please contact the BIRS team:
Tel: 01296 255670 (Mon-Fri 8:30-18:30), (Weekends and bank holidays 9:00-16:30).
Ring the BIRS team or NHS 111 as soon as possible if you experience any new or an increase in any of the following Covid-19 symptoms:
- Feeling breathless or difficulty breathing, especially when standing up or moving.
- Severe muscle aches or tiredness, shakes or shivers.
- Your blood oxygen level is 94%, 93% or consistently lower than your usual reading and you feel unwell.
- You sense that something is wrong (general weakness, severe tiredness, loss of appetite, passing urine much less than normal, unable to care for yourself – simple tasks like washing and dressing or preparing meals).
You should tell the NHS 111 operator you might have coronavirus if you have not had a positive test result.
You should attend A&E as quickly as possible or call 999 immediately if your blood oxygen levels are 92% or less:
- You are unable to complete short sentences when at rest due to breathlessness.
- Your breathing gets suddenly worse.
OR if you develop these more general signs of serious illness, for example:
- You cough up blood.
- You feel cold and sweaty with pale or blotchy skin.
- You develop a rash that does not fade when you roll a glass over it.
- You collapse or faint.
- You become agitated, confused or very drowsy.
- You stop passing urine.
- You should tell the operator you might have coronavirus if you have not had a positive test result.
A minority of people with Covid-19 will experience these more severe symptoms. These require urgent medical attention.
Please tell the Paramedics and Hospital Team that you are currently under the care of the BIRS Team.
