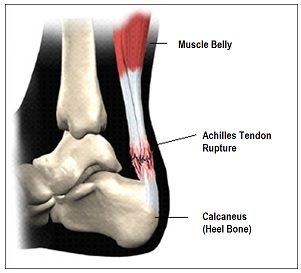
Ankle Achilles tendon full tear
Information to explain the ongoing management of your Achilles injury.
Your case history and scans have been reviewed by an Orthopaedic Consultant (Bone Specialist) and a Senior Fracture Clinic Physiotherapist.
You have sustained a rupture to your Achilles tendon, confirmed by ultrasound scan.
Healing:
This soft tissue injury normally takes about 9-12 weeks to heal.
Pain and swelling:
Take pain relief as prescribed: it is likely to be painful for several months.
Swelling is often worst at the end of the day. Elevating the foot will help.
Using your ankle:
You must use the boot with the wedges until we confirm the diagnosis. Ensure the wedges are underneath the grey liner of the boot.
Keep the boot on day and night/in bed. Do not put any weight on your foot (for example standing or walking on it) unless advised by the team.
Avoid any temptation to stretch the calf or weight bear without the boot as this could mean the tendon heals in an elongated position, which will affect your overall rehabilitation.
Personal hygiene:
You must remove your boot and sock daily to check the skin on your foot for any soreness that may be caused by excessive pressure or tightness.
You may remove the boot carefully for washing and changing your sock once a day. You must keep the toes pointed down when doing this, as demonstrated in the picture. If you want to shower, cover the boot with a polyethylene carrier bag/waterproof cover and be cautious, DO NOT remove the boot to shower.
You may remove the boot carefully for strip washing and changing your sock once a day.
You must keep the toes pointed down when doing this, as demonstrated in the picture.

Follow up:
You will be seen by a Lower Limb Specialist within 2 weeks of your injury.
Picture of injury (below):
If you have not received an appointment within 1 week of receiving this information or if you are unable to follow the rehabilitation plan outlined below or if you have any urgent questions then please contact a member of the Fracture Care Team either by phone 01296 255 630 or by email: bht.fractureclinic@nhs.net
Please follow this rehabilitation plan
What to expect:
| Weeks since injury | Rehabilitation plan |
| 0-4 |
|
| 4-6 |
|
| 6-8 |
|
| 8-12 |
|
Advice for a new injury
Rest and Elevation
Try to rest the leg for the first 24-72 hours to allow the early stage of healing to begin.
Raise your ankle above the level of your hips to reduce the swelling.
You can use pillows or a stool to keep your leg up.
Smoking advice:
Medical evidence suggests that smoking prolongs soft tissue healing time.
In extreme cases it can stop healing altogether.
It is important you consider this with your recent injury.
Stopping smoking during the healing phase of your injury will help ensure optimal recovery.
Stopping smoking during the healing phase of your injury will help ensure optimal recovery.
Follow advice on how to quit smoking on the NHS website or discuss this with your GP.
Boot advice
Diabetic patients
If you have diabetes, please contact us to discuss your boot. This is particularly important if you have problems with your skin. We can provide you with a specialist diabetic boot if required.
Footwear for your uninjured foot
We recommend choosing a supportive shoe or trainer with a firm sole for your uninjured foot.
You will notice that the boot you have been given has a thicker sole: by matching this height on the uninjured side you will reduce any stress on your other joints. You can do this by getting a shoe balancer available online; this fits easily to the shoe on your un-injured foot.
Use the crutches you have been given in the Emergency Department to help you walk.
YouTube video on using crutches:
https://www.youtube.com/watch?v=EUBiwexUnQU
Rehabilitation plan
The Team will guide you through the Rehabiliation Process and you will start Outpatient Physiotherapy at around 8-10 weeks post injury as necessary
Information on Deep Vein Thrombosis (DVT) risk and Dalteparin injections:
Due to the nature of this injury, and its rehabilitation, it is important you immobilise the foot in a boot. This places you in a higher risk group for developing a DVT (blood clot), which could potentially have very serious effects.
You may have been prescribed a course of Dalteparin/Fragmin, to thin your blood. If you have been prescribed Dalteparin/Fragmin, one of the nurses will have shown you the injection technique and you should try to keep these injections to a regular time of day.
Once your ultrasound scan results have been reviewed
We will advise you if you need to continue Dalteparin/Fragmin. If you have any further questions regarding this, or have a reaction to the medication, please direct this to your GP or district nurse.
Used injection syringes MUST be disposed of safely in the yellow ‘Sharps Bin’ provided. Once full, sharps bins can possibly be collected from your home by applying for a collection on the Buckinghamshire Council Website, otherwise the clinic team can advise as can the Pharmacy Department in the Trust. It is also possible that your GP surgery may accept these providing the lid (s) are taped down securely and put in a sealed bag.
