Pelvic girdle pain (PGP) in pregnancy
Read our guide below to find out more about pelvic girdle pain and exercises you can do to help.
You can also download a PDF version of this patient information by following the link on the right.
This information covers the most common symptoms that you might have but it isn’tt comprehensive. If you have other symptoms and want to ask anything else, speak to your community midwife.
What is pelvic girdle pain?
Pregnancy-related pelvic girdle pain (PGP) is common. Around 1 in 5 pregnant women experience it.
This may be pain at the front or at the back. For some women this lasts a short time and soon goes. For others it can be more painful and effects their movement.
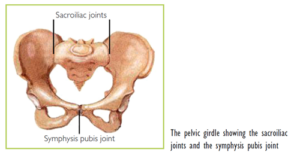
Diagram showing the sacroiliac joints in the pelvic girdle
For the majority of cases it will soon settle after your baby’s born. But as your baby grows in the womb, the extra weight and the change in the way you sit or stand will put more strain on your pelvis. You must get advice from a physiotherapist on your postnatal recovery.
What causes pelvic girdle pain?
Usually there are a number of causes which can include:
- hormonal changes in pregnancy
- increased weight on the pelvis in pregnancy
- weakness in the pelvic floor or core tummy muscles
- a pre-existing back/hip/pelvic injury
- increased BMI
- increased mobility in your joints.
If you’ve had PGP, you’re more likely to have it in a future pregnancy.
What are the symptoms of pelvic girdle pain?
The most common areas of pelvic girdle pain include:
- the front pelvic bones
- down the inside of your thighs
- in your back/buttock/hip/thighs.
Other symptoms include:
- difficulties with walking in extreme cases
- difficulty rolling over in bed because of pain
- not being able to squat
- pain when getting in and out of a car.
How can I reduce pelvic girdle pain?
During pregnancy you may find it helpful to:
- keep as active as you can within your limits but take regular breaks
- rest more frequently with your feet up, or sit down for activities that normally involve standing
- sit down to dress, for example, putting on socks/shoes and trousers
- lie on the less painful side to sleep and put 2 pillows between the knees to keep your pelvis in line with your knees
- keep the thighs as close together when changing position, for example getting out of the car.
You can also:
- ask for help with physical tasks at home and at work if you need it
- plan your day. Bring everything you need downstairs in the morning to save multiple trips up and down the stairs
- apply a cold pack to the painful bony joints and a heat pack to tight sore muscles
- take shorter steps when walking.
Physiotherapy
Get a referral to a physiotherapist. They’ll do a full assessment and advise you on a suitable individualised treatment plan. The most common treatment plan involves exercises and advice on how to move your joints. Treatment plans can vary between antenatal and postnatal women.
What should I avoid?
This includes:
- sitting cross-legged or standing on one leg
- reaching, pushing or pulling to one side
- lifting heavy weights
- bending and twisting to lift or carry anything on one hip, for example, toddlers
- positions or activities where your legs are wide apart.
When climbing stairs, try putting a basket at the top and bottom of the stairs so you can take more than one item up at a time. Go upstairs one leg at a time with the most pain free leg first and the other leg joining it on the step.
Exercises that can help
Suitable types of exercise include walking, swimming and exercise classes designed for pregnancy (such as antenatal yoga or Pilates).
Core co-contraction exercises
Your core consists of your diaphragm, deep tummy muscles and pelvic floor. Before pregnancy, these muscles automatically work together without having to think about them. In pregnancy, these muscles get stretched, weakened and can become disconnected. It’s important to keep them working together as these are the muscles that give the back, hips and pelvis the support they need.
Breathing
Practice breathing into your diaphragm.
Start by lying down. Imagine your belly is a balloon.
As you breathe in through your nose air will fill up your tummy and your belly should expand.
As you exhale through your mouth the air is being squeezed out and your belly should deflate.
Practice this and when you feel confident with the technique try it again when sitting and then standing.
Link your breath with your pelvic floor.
Breathe into your belly to prepare and as you exhale contract your pelvic floor. When you have mastered this lying down, progress to sitting and then standing. Using this technique will make sure your core is working as well as it can to support you with the movements you need to be doing daily.
Pelvic floor exercises
Try to do your pelvic floor exercises regularly. Aim for 10 second holds, 10 repetitions and then 10 quick squeezes, 4 to 6 times a day.
Start by tightening your back passage, then pull upwards as though you are stopping the flow of urine. Keep your breathing relaxed and try not to let your legs or bottom muscles join in.
Start by lying down, but progress into sitting and standing as your strength improves. You should always be able to feel your pelvic floor muscles contract and relax.
If any exercise causes pain, then limit or stop it.
Labour and birth
Most women with PGP can have a normal vaginal birth. Many women worry that the pain will be worse if they go through labour. This isn’t usually the case when you take good care to protect the pelvic joints from further strain or trauma. Tell your midwife that you have PGP.
It’s a good to have an awareness of how far you are can part your legs (abduct) before you come in to have your baby. It’s important to keep within this range as much as possible, especially if you have an epidural and cannot feel any pain due to PGP (which would otherwise warn you not to part your legs too wide).
Sometimes, for the safety of baby and for reasons not to do with your PGP, you may need an assisted birth (using forceps or a ventouse cup). In these cases you’ll need to have your legs wide apart for the birth. Everyone helping in your birth will do their best to try not to move your legs too far apart.
Before the birth
Think about birthing positions that are likely to be comfortable for you and record these in your birth preferences. Consider discussing the option of using the birth pool for labour. This
allows you to move freely and change positions easily. If you’re able to get in and out of the pool on your own, this is a safe option for you.
During labour
Use gravity to help the baby to move downwards. Stay as upright as possible in positions including:
- kneeling
- on all-fours
- standing.
These positions allow labour to progress and avoid further strain on your pelvis.
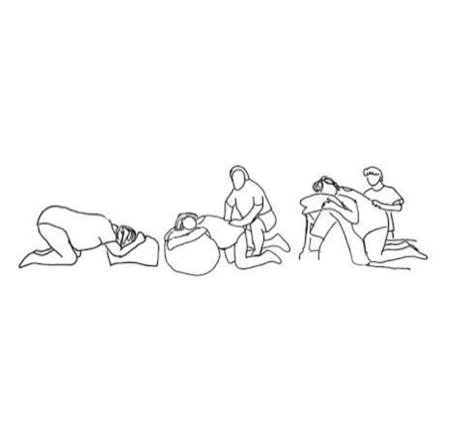
Positions for labour
Try to avoid lying on your back or sitting propped up on the bed. These positions reduce the pelvic opening and may slow labour.
You should never put your feet on the midwife’s or your partner’s hips when pushing to deliver your baby. It may put too much strain on your pelvic joints and may also damage the back of the person supporting you.
You may be able to lie on your side for internal examinations. Ask your midwife or doctor about this.
Useful information
Find out more about managing pelvis girdle pain in pregnancy
How can I help reduce healthcare associated infections?
Infection prevention and control is important to the wellbeing of our patients so we have procedures in place. Keeping your hands clean is an effective way of preventing the spread of infections.
You, and anyone visiting you, must use the hand sanitiser available at the entrance to every ward before coming in and after you leave. You may need to wash your hands at the sink using soap and water. Hand sanitisers are not suitable for dealing with patients who have symptoms of diarrhoea.
About our patient information
This is intended as general information only. We aim to make the information as up to date and accurate as possible, but it’s subject to change.
Always check specific advice on any concerns you may have with your doctor.
Contact us
01296 315000
01494 526161
