Blood Clots: Reducing the Risk
Information on how you can reduce the risks of deep vein thrombosis (DVT) and pulmonary embolism (PE) during and after your stay in hospital.
What are blood clots (VTE)?
Your blood has a mechanism that normally forms a blood clot (plug) to stop the bleeding when you are injured (example: when you have a cut). Sometimes this mechanism can go wrong and a blood clot forms when there is no injury, which can block the vein and stop blood flowing to the affected area.
This is called venous thromboembolism (VTE), which can happen:
In a vein of the leg causing a deep vein thrombosis (DVT)
If the DVT becomes loose, it can travel to the lungs causing a pulmonary embolism (PE). This condition can be fatal.
DVT can lead to post-thrombotic syndrome on the leg (permanent pain, difficulty walking, leg wounds that don’t heal). PE when not fatal, can lead to chronic pulmonary hypertension (weak heart, chest pains, shortness of breath).
Anyone can have VTE! Including you! Even if you are fit and healthy.
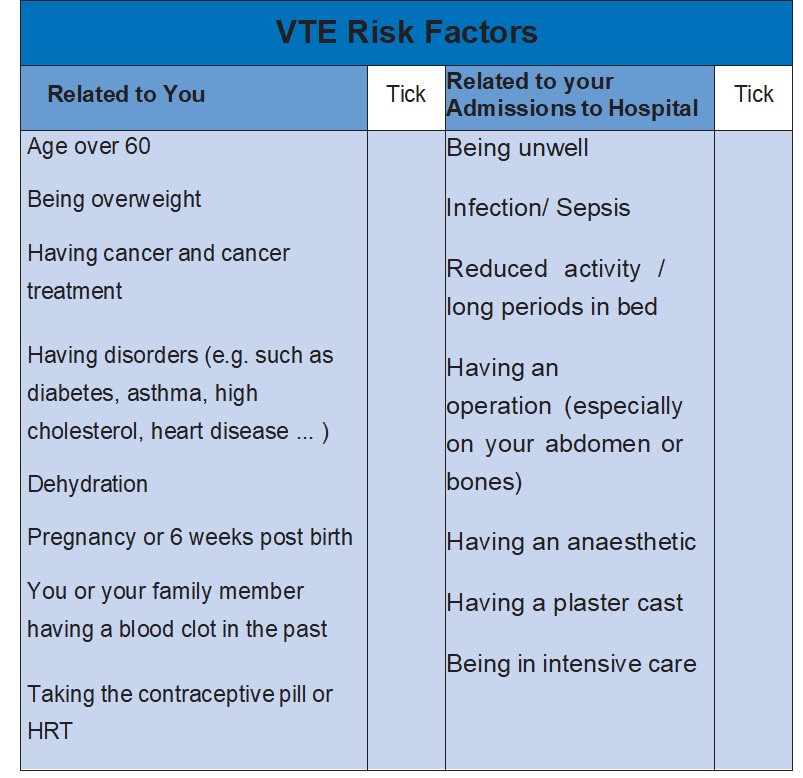
Who is more likely to have VTE?
If measures are not in place to prevent VTE, up to 40% of patients admitted to hospital will develop a DVT but it could be as many as 60% in orthopaedic (bone) surgery.
The risk varies from patient to patient so all patients admitted to hospital should have an assessment for their risk of developing a VTE.
The following table shows a list of conditions that make you more likely to have VTE. Do you have any of them?
How to reduce the risk of VTE
- Stay active
- Drink plenty
- Do VTE prevention exercises
VTE Prevention Exercises
Always check with your doctor if it is safe for you to do these exercises. They increase the blood flow to the legs and lungs helping to prevent VTE during your hospital stay.
Do 10 repetitions of each exercise every hour.
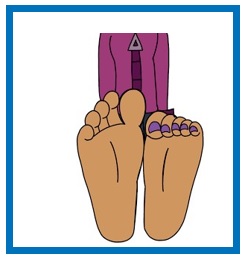
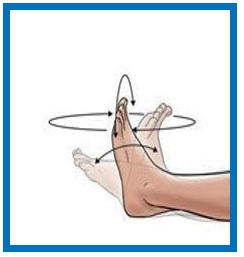
Leg exercises
Paddle your feet up down and circle them around and around. The circle motion should be clockwise and then anticlockwise.
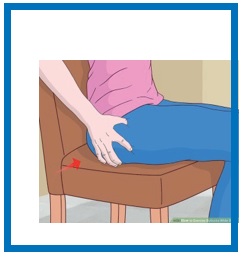
Buttocks squeezing Lying down or sitting, clench your buttock muscles together and hold for a count of 3 before relaxing.
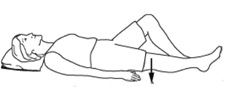
Static Quads and lifts Lie down, with kneecap and toes facing the ceiling. Tighten the muscles in the front of the thigh and push the back of your knee into the bed holding for 3 seconds and then relax.
Static Quads and lifts To do the lift, raise your leg from the bed with the knee held straight, hold it for 3 seconds and gently bring the leg down.
Knee bends and lifts Hold on to a table or counter for support. Slowly bend your knee by lifting your heel towards your buttocks. Hold for 3 seconds. For the lifts slowly raise your knee up to the level of your hip, hold for 3 seconds. Slowly lower your foot to the floor.
Sit to standing: Sitting on a chair, holding on to a table or counter, stand up and sit back down slowly, keeping your back straight.
Breathing exercises
Place your hands on the side of your rib cages.
Take a slow deep breath and feel the ribs being pushed upwards and out to the side as you expand your lungs. Hold it for 3 seconds. Breathe out slowly with your lips closed together as if you are whistling.
How to reduce the risk of VTE? By doctor’s prescription:
- Antiembolism stockings and leg cuffs
- Medication (injection or tablets)
Heparin type medicines are from animal origin
(example: Dalteparin / Fragmin).
If your personal beliefs set restrictions on the consumption of animal products, or you are vegetarian or vegan, discuss with your doctor or nurse.
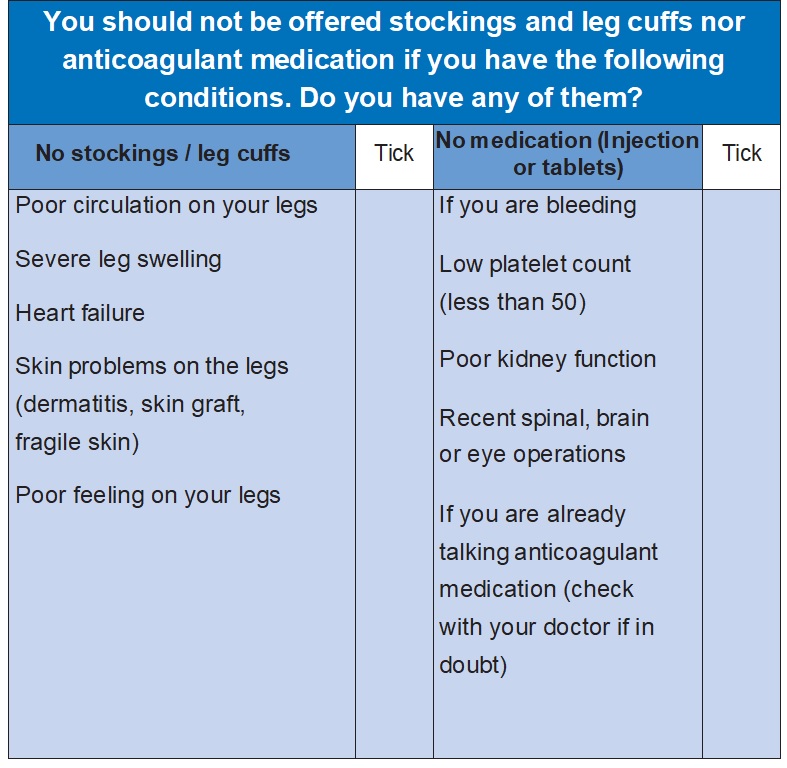
What if I can’t have the treatment?
If you have risk factors and have not been given stockings, leg cuffs and/or medication to prevent VTE you may not be able to have them. Check with your doctor to be sure.
Are there possible complications of treatment?
Most complications are mild and reversible.
Antiembolism stockings and leg cuffs
If you are wearing an incorrect size or if they are ill-fitting, the following complications can happen:
- Skin marks
- Wounds or blisters
- Discomfort
This is more common with stockings than leg cuffs.
If this happens in hospital, let your nurse or doctor know as soon as possible. If you have been discharged please call your GP as soon as possible.
Stockings or leg cuffs should only be stopped upon advice from your doctor.
How to avoid complications
- Both legs should be measured to determine the stockings’ size
- When wearing them, the heel landmark should be centred on the heel
- Stockings not rolling down the leg, not wrinkled, not folded over, not pulled high above the knee or folded back over the toes
- Remove them every day to check legs and feet for marks or redness leaving the stockings off for a maximum of 30 minutes to avoid interruption in blood clot prevention
- Remove them if you find any red areas or wounds and in form the doctor or nurse straight away, they will tell you what to do.
Medication (injection or tablets)
- Allergy (e.g. rash)
- Bruises
- Bleeding (e.g. nosebleeds, blood in the urine or stools, from surgical wounds, heavy periods, internal bleeding)
- Extreme tiredness
- Pallor
If this happens in hospital, let your nurse or doctor know ASAP. If you have been discharged please call your GP ASAP. Medication should only be stopped upon advice from your doctor.
How do you know if you have VTE?
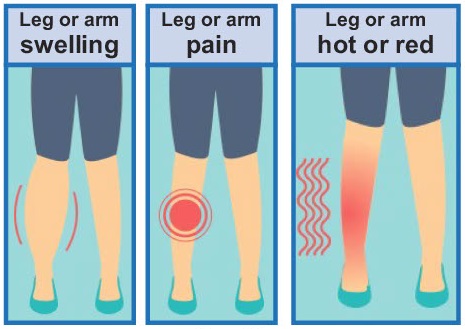
DVT requires urgent care.
If you experience any of the symptoms show in the images above while you are in hospital let your nurse or doctor know as soon as possible. If you have been discharged please call your GP as soon as possible.
Signs and symptoms of pulmonary embolism
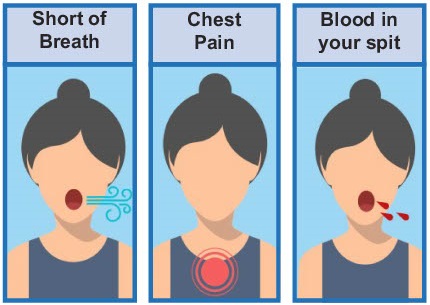
Pulmonary embolism (PE) is an emergency!
If this happens in hospital, let your nurse or doctor know immediately. If you have been discharged.
Call 999 straight away.
Advice for when you leave the hospital
You will still be at risk of getting VTE up to 3 months after leaving the hospital. In fact, most blood clots appear after leaving the hospital.
That is why it is so important to keep following the general advice about “How to Reduce the Risk of VTE” in this leaflet. In addition to that, the doctor may prescribe you antiembolism stockings and / or medication to go home with.
If you are discharged with antiembolism stockings:
This is common if you had major surgery, if you had VTE in the past, if you have other significant VTE risk factors or if you will have ongoing reduced mobility after discharge.
- Ask your nurse what your leg measurements and stocking size are – calf width __, leg length __ , size __.
- Ask your doctor how long you should wear the stockings for (days/weeks?).
- Make sure they fit correctly (heel pocket on the heel, not rolling down or folded, not hurting. The stockings should provide a firm, even pressure).
- Wear them all day and all night
- Always remove the stockings every day for no longer than 30 minutes this is essential to check for complications (see section ‘Are There Possible Complications’).
- Wash the stockings every 2-3 days or when dirty: hand or machine wash with cold water on a delicate cycle. Hang or lay flat to air dry. You will need 2 pairs to be able to wash them while wearing the other pair.
- Remove them and inform your GP if you have any issues or complications.
If you are discharged with anticoagulant medication:
This is common after bone surgery or fracture, gynaecological surgery, major surgery, if you have had COVID19, if you have had surgery to remove a cancer or if you had a previous VTE. It may be required in other situations as well.
- Make sure you take it as prescribed
- Take it every day at the same time/times
- Do not miss any doses
- Keep an eye out for bleeding (see section ‘Are there any possible complications’ on this leaflet)
- If you have any problems with your anticoagulant medication, contact your GP immediately
- If your medication is in the form of injection you will be asked to give it to yourself if you are able to. You should be shown how to do the injection and ideally try it yourself before going home. You must be given the leaflet “Dalteparin prefilled syringes. How to administer Dalteparin at home: A Patient Guide”
Dalteparin injection:
- The injection is ready to use, no fiddling about
- The needle is one of the smallest (1.2 cm long)
- The liquid to inject is also very little (0.2 ml)
- The injection procedure is easy
- It feels like minor stinging
- It only takes about 20 seconds
- Alternative arrangements are available if you can’t do it
Information about Dalteparin is available on our website.
Useful information:
- Trust Patient medicines helpline: 01296 31 6197
- Information for patients on our Trust website
- Venous thromboembolism in over 16s: reducing the risk of hospital-acquired deep vein thrombosis or pulmonary embolism
- NHS information about blood clots
- Download the Preventing VTE app